by editor | Mar 22, 2023 | Compliance and Regulatory - Directors, Metrics and KPIs, Rules and Regulations - Nurses, Rules and Regulations - Office Team
Patient length of stay is monitored to detect instances of inappropriate use of the hospice benefit or other deficiencies in the services delivered by the hospice provider. Length of stay is monitored for both very short length of stay as well as for length of stay that is longer than the norm.
What may unusual length of stay tell a hospice provider?
When patients are discharged alive with a short length of stay it may signal that the patient did not understand the hospice benefit when the patient was admitted to hospice. Or, patients may discharge live from hospice after just a few days because they were not satisfied with the services delivered by the hospice provider. Patients with length of stay longer than 180 days could be indicative of a patient who is no longer hospice eligible. Patients who are no longer eligible for service should be discharged from hospice and any payments that were received from Medicare while the patient was no longer eligible for services should be returned to Medicare. Failure to discharge the patient or failure to return the funds are examples of fraud and abuse.
How is length of stay calculated?
Length of stay is calculated based on the number of days that a patient receives hospice care. Specifically, for a patient who is discharged from hospice (whether or not the patient is discharged alive), the patient length of stay is calculated as follows:
Patient length of stay = [patient discharge date]-[patient admission date]+1
Which patients are included in length of stay calculation?
The length of stay calculation assumes that only discharged patients are considered in the calculation – since the formula expressly refers to the patient discharge date. When only discharged patients are considered (whether live discharges or discharges due to death), the hospice provider only has a backward-looking view on performance relating to length of stay. For example, if a hospice provider has been providing service to a patient for 12 months and the patient is still on service, the patient will not be included in the traditional average length of stay metric – since the patient has not yet been discharged. On the other hand, once the patient is discharged the patient’s length of stay will be at least 365 days since the patient – while still currently active – has already been on service for 365 days. If active patients are considered in a length of stay calculation, it gives a hospice provider a metric that can be used to highlight patients whose clinical charts and documentation of care may benefit from additional review.
What length of stay metrics should be calculated?
In addition to computing average and median length of stay based on discharged patients only, average and median length of stay can be computed for active patients. Patient length of stay for an active patient is calculated as follows:
Active patient length of stay = [end of evaluation period date]-[patient admission date]+1
For example, suppose the current date March 15, 2023 and a hospice wishes to calculate the active patient length of stay as of the end of 4Q 2022 for a patient who was admitted on December 1, 2022. The calculation is as follows:
- End of evaluation period date: 12/31/22
- Patient admission date: 12/1/22
- Active patient length of stay = (12/31/22) – (12/1/22) + 1 = 31 days
The active patient length of stay as of the end of 4Q 2022 is 31 days.
If the hospice wishes to calculate the active patient length of stay as of current date, the calculation is as follows:
- End of evaluation period date: 3/15/23
- Patient admission date: 12/1/22
- Active patient length of stay = (3/15/23) – (12/1/22) + 1 = 105 days
Average and median length of stay would be computed as usual. If any concerning value — such as long length of stay – is identified based upon the active patient length of stay, a hospice provider can immediately investigate and determine if any remediation action is required, rather than waiting until patients are discharged. Delay can lead to additional fines or further action from Medicare.
by editor | Mar 22, 2023 | Compliance and Regulatory - Directors, Metrics and KPIs, Rules and Regulations - Nurses, Rules and Regulations - Office Team
Patients are eligible for hospice if they have a terminal diagnosis and a prognosis of six or fewer months to live if their disease runs its natural course. A patient who lives longer than six months can still get hospice care if the medical director or other hospice physician recertifies that the patient is still terminally ill.
What is hospice patient length of stay?
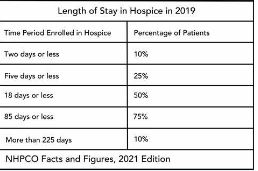
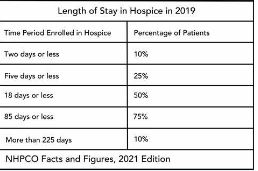
Hospice length of stay is an important metric that is monitored by both CMS and by hospice providers. Hospice length of stay measures the count of days that a patient receives hospice services, from the day that the patient is admitted into hospice until the day the patient is discharged (either alive or deceased). In 2018, 25% of Medicare beneficiaries received hospice care for seven days or less and 54% of Medicare beneficiaries received hospice care for 30 days or less.
Why should a hospice monitor patient length of stay?
Monitoring patient length of stay can aid in detecting cases of possible fraud or abuse – instances where ineligible patients continue to receive the hospice benefit. This metric also helps monitor whether the hospice benefit is being adequately utilized. Although patients are eligible for hospice when they have six months or less to live, most patients receive less than 30 days of hospice care.
Agency patient length of stay is also trended over time and is also compared against the value for patients in the same region, state, or nationwide. The metric may also be analyzed for patients in subpopulations – for example patients with the same disease, race, or ethnicity.
How is patient length of stay calculated?
Patient length of stay is calculated using all patients discharged by the hospice provider during the reporting period. For example, if the hospice would like to compute the length of stay for patients during the 4Q 2022, all patients who were discharged during 1Q 2023 would be included in the calculation. For each patient, the number of days from the date of patient admission until the date of patient discharge is counted; this represents the patient length of stay.
Patient length of stay = [patient discharge date]-[patient admission date]+1
What are common measures of length of stay?
Two common patient hospice length of stay measures are Average Length of Stay (ALOS) and Median Length of Stay (MLOS).
Average length of stay
Average length of stay is the arithmetic mean of the data collected. Specifically, if d is patient length of stay and N is the total number of patients then average length of stay (ALOS) is calculated as follows:
ALOS = ( d1 + d2 + d3 + …. + dn ) /N
Where di = patient length of stay for patient i
Median length of stay
Median length of stay is the middle number in the sequence of numbers. Specifically, compute the length of stay for all N patients. Then, order these N numbers in ascending order. The middle number is the median. If the number of patients is even then there is no middle number. Instead, the median is calculated by taking the average of the two numbers in the middle.
Comparing average and median length of stay
The average is sensitive to outliers in the data. That is, if there are a few patients with a very high length of stay while all other patients have a significantly lower length of stay, the average will be biased by these outliers and will give a misleading assessment of overall patient length of stay. Below, we give an example to provide greater intuition into the impact of outliers on average length of stay and the difference between mean and median length of stay.
Suppose a hospice agency discharged 35 patients during 4Q 2022. The patients’ lengths of stay are as follows:

We compute the average length of stay by summing each of the 35 patient’s length of stay (in the “Length of Stay” column) and dividing that total by 35 (the total count of patients).
Average length of stay (ALOS) = 38.5
We compute the median length of stay by sorting the patient’s length of stay in ascending order and identifying the central number. Since there is an odd number of patients, there will be a single central value. In this case, the central value is 20.
Median length of stay (MLOS) = 20
Average length of stay is almost double the median length of stay. What is leading to these significant differences between ALOS and MLOS? Observe the outliers in the data. There are two patients with length of stay that exceeds 200 days. There are two additional patients with length of stay exceeding 100 days. Since ALOS is sensitive to outliers, ALOS is being pulled to a higher value due to the presence of these outliers.
To provide additional insight, we have plotted a histogram of the length of stay values. A histogram shows the count of observations in the data that fall in each of the specified ranges.

The table on the left shows the count (frequency) of observations of patient length of stay in the data for each of the ranges: 0-10 days, 10-20 days, 20-30 days, 30-40 days, and greater than 40 days. There are 11 patients with length of stay between 0-10 days, 7 patients with length of stay between 10-20 days, 6 patients with length of stay between 20-30 days, 6 patients with length of stay between 30-40 days, and 4 patients with length of stay that exceeds 40 days.
Think about this histogram and now consider the MLOS and ALOS. Median length of stay is 20 days – it falls well in the middle of the data. Average length of stay, however, equals 38.5. It falls, essentially, in the final bar of this histogram and well beyond where the majority of the data lies. The provides a visual demonstration of the impact of outliers on ALOS.
Providers should monitor both ALOS and MLOS. Significant differences between these numbers would indicate the presence of outliers and should be investigated.
Print ‘n take hospice keys
- Understanding the difference between the average (mean) and the median
hospiceKeys-meanVsMedian
Where can you find out more?

by editor | Jan 29, 2023 | Compliance and Regulatory - Directors, Metrics and KPIs
Why is data valuable?
Like all other business decisions, a hospice marketing plan must be data driven. More progressive hospice agencies have increasingly begun to understand the value of many types of data in supporting business decisions. This includes internal data such as patient EMR data, financial data including general ledger revenue and expense data (at various levels of aggregation), and quality data. It also includes external data such as publicly available claims data, cost report data, and referral data.
This article published in June 2021 discusses how hospice agencies are using data analysis as a tool to gain an edge over competitors when engaging with potential referral sources. The discussion focuses on use of data analysis to identify which physicians represent referral sources that are more likely to produce (higher quality) referrals. This 2016 NHPCO article discusses the use of hospice metrics as a marketing tool. For example, a hospice agency can share statistics on reduction in hospital admissions for its patients in hospice compared to hospital admissions prior to hospice admission. Other metrics on cost of care or patient satisfaction are of interest, depending upon the referral source.
What data is valuable for designing a marketing strategy?
A hospice should gather data so that it can develop a complete picture of the customers that it serves. It should analyze its patients – including referral sources and patient attributes such as patient diagnosis, length of stay, and patient demographics. Referral sources can be analyzed at different levels of aggregations such as geographic location, facility type, physician type, and physician name. Analysis of hospice patients should be compared to analysis of data for the entire market (in the relevant geographic region). This can help a hospice agency identify where it may have strengths or weaknesses and contribute to its marketing strategy.
Analyze the data: gain input from multiple sources
When analyzing the output of the data analysis, the hospice agency should solicit input from multiple sources in the organization. Combining different perspectives on the data such as input from the executive, marketing, and clinical teams will provide a more holistic view and a more accurate assessment of the current marketing performance and how the go-forward marketing strategy should be designed.
How can the data be analyzed?
The simplest method for analyzing the data is to use Microsoft Excel. Excel is widely used in most organizations, so gaining access to this software should not be difficult. With relatively simple commands, one can analyze data and create charts to visualize the results of data analysis. Another benefit of using Excel for data analysis is that a lot of educational material is available on the Web to answer any questions that you may have about using Excel – in case there are data analysis functions that you want to learn more about.
What other information may be relevant to developing a strategy?
Patient data and claim data are historical data that are important inputs to a developing a marketing strategy. A hospice agency should also analyze forward-looking data as well as more general information such as:
- What are hospice market trends in the geographic region?
- How competitive is the marketplace and are there expectations for change in competition in the near term?
- How well is the role of hospice understood by communities in the geographic region?
- Is the use of hospice accepted by communities in the geographic region?
- Is hospice understood by the medical community in the geographic region?
- What are the demographics of your geographic region and are they expected to change in the near term?
Combining analysis of historical and forward-looking data and soliciting input from team members with different perspectives such as operational, clinical, and marketing will help a hospice agency develop an effective marketing plan.
Where can you find out more?
Using hospice metrics for marketing
by editor | Jan 29, 2023 | Compliance and Regulatory - Directors, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Office Team, Hospice 101 - Social Workers, QAPI, Regulatory Compliance
What is the governing body?
In accordance with the Conditions of Participation, a Medicare certified hospice agency must have a governing body. The governing body has ultimate responsibility for the hospice agency, including legal and financial authority. Medicare Conditions of Participation require that the governing body is informed of the ongoing activities at the hospice agency, including patient care delivery issues and all QAPI activities. The governing body must also appoint a qualified hospice administrator – a hospice employee with the necessary education and experience – who is responsible for hospice daily operations.
The governing body must meet at least quarterly and must maintain written minutes of its meetings.
There are two Conditions of Participation – 418.100 and 418.58 – that relate to the hospice governing body.
Condition of Participation 418.100
This Condition of Participation defines a standard that the governing body is responsible for management of the hospice agency, including its fiscal operations, provision of services, and continuous quality assessment and performance improvement (QAPI) efforts. The governing body also assumes full legal authority of all hospice operations. It further specifies that the governing body should appoint an administrator that reports to the governing body and who is responsible for hospice agency daily operations. The hospice administrator must be a hospice employee and must have necessary training, education, and experience. CMS does not specify the process by which an administrator should be selected by the governing body. If a hospice agency has multiple locations, the governing body is responsible for administration, supervision, and services for all locations as well as for any arranged services.
Condition of Participation 418.58
This Condition of Participation discusses requirements of a hospice agency’s QAPI program. The governing body must ensure that the hospice agency maintains and implements an ongoing quality improvement and patient safety program. Program performance must be monitored on a regular basis. Further, the governing body must ensure that one or more individuals are selected to lead the organization’s QAPI efforts.
The hospice agency’s organization documents must specify that the hospice governing body is responsible for the QAPI program. Additionally, the governing body specifies the frequency of data collection and level of detail of data collected by the QAPI program.
Are there any state regulations?
State hospice licensure regulations may impose additional requirements on the hospice governing body. They may also have specific requirements on the administrator that is selected by the governing body. A hospice is required to meet the most stringent requirements (whether state or federal).
Surveyors will check that all conditions are met. A hospice agency should maintain evidence of the governing body’s role and activities. Governing body authorizations and activities should be documented in governing body meeting minutes, company organization documents, and company policies and procedures.
Where can you find out more?
CMS Conditions of Participation – Governing Body
by editor | Jan 28, 2023 | Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Nurses, Metrics and KPIs, Rules and Regulations - Nurses
What is a UPIC?
Unified Program Integrity Contractors (UPICs) are contracted by CMS to conduct detailed medical review, data analysis, and audits of healthcare providers to investigate possibilities of Medicare or Medicaid fraud, waste, and abuse.
While the primary purpose of a RAC or MAC audit is to review payments, the primary purpose of a UPIC audit is to investigate when there is suspicion of fraud – especially fraudulent billing practices. A UPIC audit can lead to federal Medicare fraud charges or criminal prosecution. As such, UPIC audits are more serious than other audits.
What is a UPIC’s scope of responsibility?
Prior to UPICs, Zone Program Integrity Contractors (ZPICs) had been responsible for performing fraud, waste, and abuse detection and prevention activities for CMS. In 2016, CMS began to transition to the UPIC program. This transition took a number of years, with ZPIC contracts rolling over to the UPIC program as ZPIC contracts expired. The ZPIC program has now been phased out and replaced with UPICs. UPICs were formed as part of the Comprehensive Medicaid Integrity Plan (CMIP) with the intention of consolidating under a single federal contractor work performed by numerous Medicare and Medicaid program integrity contractors. UPICs combine all federally funded integrity reviews into a single audit and place payments to all federally funded payers under a higher level of scrutiny.
Consolidating responsibility provides UPICs with access to more data and information about healthcare claims, billing, and payments to hospice agencies. By increasing the level of information and data to which UPICs have access, UPICs have improved ability to identify billing anomalies and fraud.
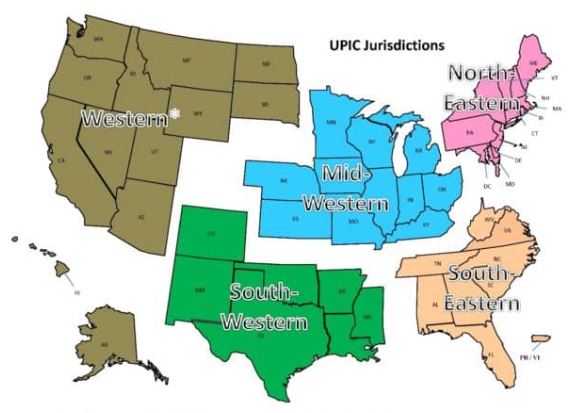
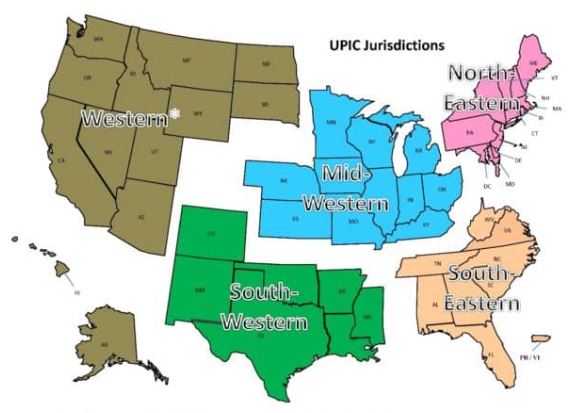
With respect to regional responsibility, the United States has been split into different geographic jurisdictions: Western, Mid-Western, North-Eastern, South-Eastern, and South-Western. Each UPIC is responsible for handling federal-level audits for both Medicare and Medicaid in one of the different geographic jurisdictions.
How is a hospice agency targeted for a UPIC audit?
UPIC audits are usually triggered by statistical analysis of hospice claims and billing data that identifies anomalies in in a hospice agency’s billing. Factors that often lead to a hospice being targeted for a UPIC audit include:
- Billing trends that are inconsistent with industry trends
- Long inpatient stay
- Referral from law enforcement or a federal agency. (For example, a hospice agency may be referred to a UPIC if at the conclusion of a MAC investigation for improper billing, the findings cannot be classified as billing errors or misunderstandings.)
- Complaints to the OIG
- Inaccurate Medicare billing
- Greater frequency of high end services as compared with local or national averages and patterns
What activities may be involved in a UPIC auditor’s investigation?
UPIC audits are focused reviews. A UPIC will request medical records and conduct interviews to determine whether fraud has occurred.. The UPIC’s audit process typically consists of a detailed review of the hospice’s records to confirm all Medicare billings. A UPIC auditor’s activities may be varied and may extend well beyond a review of medical records and documentation including activities such as:
- On site visit
- Interview hospice patients and/or hospice agency employees
- Review clinical, financial, and time production records
- Perform data analysis
- Look for prior agency violations
How does a UPIC audit progress?
A UPIC audit will typically begin with a letter requesting submission of documents – typically within 30 days but sometimes within 15 days. Most UPICs will agree to an extension of time for document submission.
A hospice agency should carefully review the nature of the request. Is the UPIC only requesting administrative and claims related medical records or is the UPIC also requesting documentation relating to the hospice agency’s business practices?
If the UPIC requests information about the hospice agency’s business practices or business relationships – such as its referral sources – this may indicate that the UPIC received information that the hospice agency is engaged in questionable business practices. If the UPIC identifies improper practices, the hospice agency will be referred to the Office of the Inspector General (OIG) or Department of Justice (DOJ).
If the UPIC only reviews claims and the associated medical or billing records, then there are typically two cases:
- Case 1 – The UPIC requests ten or fewer post-payment claims: the UPIC is likely conducting a “Probe Sample”. The purpose of a probe sample is to check if there are problems with the hospice agency’s billing practices, medical necessity, or documentation. This means that the data analyst identified a potentially problematic pattern following the data analysis. The investigator was notified of this pattern and a sample of claims is requested that match the identified pattern. If no significant problems are identified in the initial sample of claims, the UPIC typically issues an “Education Letter”. If numerous problems are found, the UPIC usually expands its audit and issues a request for a larger sample of 30 or more claims.
- The auditor will extrapolate based upon the findings of the 30 or more claims. Extrapolation allows the auditor to identify the error rate in the sample, and then extrapolate the error rate over the entire universe of six years of claims. (Six years is the maximum look back period for claims review.) For example, if the auditor collects a sample of 50 claims and errors are identified in 10 claims, then the error rate is 10/50=20%. It is then assumed that the accuracy of the billing identified in the sample is indicative of the entire universe. Consequently, the error rate of 20% identified in the sample is applied to the entire universe. Even if the hospice agency changed processes, billing software, or billing staff during the duration of time period of the universe, the sample error rate is still applied to the universe. As such, the impact of extrapolation is often quite significant.
- Case 2 – The UPIC requests 30 or more claims: the UPIC likely selected these claims as part of a “Statistically Relevant Sample” and will extrapolate the error rate that it finds to the entire universe of claims.
UPICs also conduct unannounced office visits to hospice agencies. If an office visit occurs, the UPIC will arrive at the office site with written request for patient medical records. They will also interview patients and hospice agency workers.
What may be the outcome of a UPIC audit?
A UPIC audit may result in payment suspension if there are findings that indicate the existence of overpayment, incorrect billing, or fraud.
When a hospice agency is faced with payment suspension, it may follow the standard Medicare appeals process. Legal counsel may be helpful in guiding a hospice agency regarding rights as applied to recoupment and claims withholding.
Payment suspension sometimes occurs without prior notice to the hospice agency. If the agency receives prior notice, it has 15 days to rebut. The UPIC must respond within 15 days of receiving the rebuttal. CMS then determines if the suspension should be removed. In most cases, the suspension remains in place.
Initial payment suspension can last up to 180 days with two unappealable 180 day extension periods.
A hospice may continue to provide services and submit claims while payments are suspended. During the suspension period, payments are not made to the hospice. Instead, payments are made to an escrow account that is managed by the UPIC.
If overpayments are identified, they are taken from the escrow account. The balance remaining in the escrow account is returned to the hospice agency once the audit is completed.
If the UPIC identifies any fraudulent behavior, the activity is referred to the Department of Justice (DOJ) or to the Office of Inspector General (OIG).
What if a hospice agency disagrees with UPIC findings?
A hospice agency may appeal overpayments identified by the UPIC through the Medicare administrative appeals process.
How can a hospice agency prevent UPIC audits?
By increasing their compliance efforts and activities, hospice agencies can prevent UPICs and decrease the chance of a negative outcome from a UPIC audit. More specifically,
- CMS requires that every hospice agency have a compliance team. In addition, compliance reporting duties must be defined.
- A hospice’s compliance plan must be kept current and should include
- How to update coverage guidelines from CMS
- Billing protocols
- Staff hiring and training on protocols
- Documentation guidelines
- HIPAA information and training
- Protocols for cross checking Medicare and Medicaid claim data
- Hospice compliance teams should conduct periodic and random internal audits of patient records, billing documentation, and required signatures. Compliance teams should look out for persistent errors and indications such as is additional biller training is required – either for the team or for a specific biller? Or, is there a new regulation that the team is not familiar with? Is there a physician who is consistently late with signatures? A clinician whose documentation does not look complete or timely? Charts should be audited randomly but on an ongoing basis and indications of the need for self-disclosure should be followed up on. Self-disclosure results in overpayment, but it typically removes a hospice agency from being a target for UPIC audits since it is an indicator that the hospice conducts internal self-audits and returns overpayments, as necessary.
- Hospice agencies can hire third party auditors to conduct chart and coding audits. These third-party auditors can suggest improvements to billing processes or hospice operations to improve compliance with regulations.
- Track all payer document requests and reimbursement denials; these may help identify billing problems before they are identified by an auditor.
Where can you find out more?
by editor | Jan 28, 2023 | Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Nurses, Metrics and KPIs, Rules and Regulations - Nurses
What is a TPE?
A Targeted Probe and Educate (TPE) is an audit program that was rolled out by CMS in 2017. The stated goal of this program is to help providers reduce claim denials and appeals. The TPE works to achieve its goal by educating providers in topics that will help to eliminate common mistakes that lead to recoupment of Medicare payments.
Through the TPE program, CMS (through the MAC) works directly with the hospice agency to identify errors and
- Assist or direct in correcting the errors
- Assist to quickly improve when errors are found
- Provide one-on-one help or education
TPE audits are not random spot checks. They are targeted audits. A hospice is identified based upon MAC data analysis or claim review. A hospice with high error rates or unusual billing practices may also be selected for a TPE. TPEs often focus on items with high national error rates. TPEs also focus on items that pose financial risk to Medicare.
TPEs target hospice agencies that fall within these identified risk categories. A hospice agency that is compliant with Medicare policies and billing practices will not be selected for a TPE.
What is the TPE audit process?
The TPE audit process begins with a Notification Letter sent from the MAC to the hospice agency. The Notification Letter explains the TPE program and informs the hospice agency that it has been selected for a TPE audit. It also explains the reason that the agency was included in the TPE and advises that an additional documentation request (ADR) is forthcoming. No response to the Notification Letter is required.
TPE Round 1
The ADR arrives following the Notification Letter. The ADR includes a list of 20-40 claims for which medical records and documentation supporting the claims are requested. This is considered Round 1. The hospice agency must submit the requested documentation.
The MAC reviews the documentation supporting the 20-40 claims to determine if the documentation supports the claims that were submitted.
If the hospice agency is deemed compliant (“no unfavorable findings”) after review of the documents submitted in response to the ADR in round 1,
- Round 1 ends
- No further reviews on that topic for at least one year
If there are unfavorable findings (issues are noted):
- One-on-one educational sessions are offered to the provider
The hospice should participate in the one-on-one education. This education provides the hospice agency with an opportunity to speak directly with the auditor and discuss the errors identified. During these sessions, the MAC guides the hospice agency through error correction. Following the education there is a 45 day period for the hospice to make improvements (e.g., system improvements, process improvements) before another TPE review by the MAC. If the MAC is satisfied that the errors have been corrected, the audit is closed. However, if more errors are identified the hospice agency will be entered into another audit round.
TPE Round 2
A second ADR is sent requesting another 20-40 claims. The hospice agency submits the documentation which is again reviewed by the auditor. The process followed in TPE Round 1 repeats. If there are unfavorable findings, the TPE advances to Round 3.
TPE Round 3
A third ADR is sent requesting another 20-40 claims. If there are still unfavorable findings in Round 3, the hospice agency is referred to CMS for next steps including:
- Shift to 100% prepay review
- Referral to a RAC
- Extrapolation/recoupment
- Other action, as instructed by CMS
What is the MAC looking for in the TPE audit?
During the TPE audit, the MAC is looking for billing mistakes that cause hospice agencies to be non-compliant with regulations. The most common problem identified during a TPE audit is that the documentation does not support terminal prognosis of six months or less.
What if a hospice agency disagrees with the audit findings?
If a hospice agency disagrees with the audit findings, the agency can appeal the results through the Medical Appeals Process. The hospice agency will need to request a redetermination of overpayment by the MAC.
Where can you find out more?