by editor | Aug 25, 2024 | Care Keys - Aides, Care Keys - Chaplains, Care Keys - Nurses, Care Keys - Social Workers, Rules and Regulations - Office Team, Rules and Regulations - Social Workers, Rules and Regulations - Volunteers
As a member of the hospice healthcare team, you play an important role in caring for your patients. Because of this, you will often learn private information about them – not just about their health, but also about their personal relationships, their financial situations, and other sensitive and personal information. It is important to understand that you have a legal and ethical responsibility to keep this information confidential and only share it – when necessary – with other healthcare professionals who are part of the patient’s care team. It is your responsibility to protect patient privacy.
Why is it important to keep healthcare information private?
In 1996, the Health Insurance Portability and Accountability Act (HIPAA) was passed to protect people’s health information. The main goal of HIPAA is to ensure that health information is kept private and secure, and only shared with those who need to know in order to provide care or process medical records. This law applies to everyone working in healthcare.
What does HIPAA protect?
HIPAA protects what is called “personal health information” (PHI). This includes any details that could identify a patient, such as:
- Name
- Medical record number
- Date of birth
- Address
- Email address
- Social security number
Only those directly involved in a patient’s care or those who handle billing or administrative tasks should have access to this information.
Your role as a member of the patient’s healthcare team
As a member of the patient’s healthcare team, it is important to follow HIPAA rules to protect your patient’s privacy. If you share a patient’s health information without permission, it can harm the patient and break the trust they have in you. Here are some important things to keep in mind:
- Do not share information unnecessarily: Never discuss a patient’s health with friends, family, or on social media. Only discuss patient care with other healthcare workers who are directly involved in that patient’s care.
- Keep conversations private: If you need to talk about a patient’s care with another healthcare worker, make sure you do so in a private place where others cannot overhear.
- Secure patient records: Whether you are handling paper records or using electronic systems, always ensure that patient information is stored securely.
Why following HIPAA is important
By following HIPAA regulations, you help protect your patient’s privacy, ensure their information is handled with respect, and build trust. Patients and their families rely on you to keep their personal information safe, and HIPAA provides the guidelines you need to do so.
What are the guidelines of not following HIPAA?
Hospices and their employees must protect patient information at all times. If HIPAA rules are not followed, it can lead to serious consequences including fines, penalties, and even imprisonment. This applies not just to the hospice itself but also to any vendors or contractors who work with patient information.
Final thoughts
Understanding and following HIPAA is an essential part of your job as a member of a patient’s healthcare team. By keeping patient information private, you help ensure their safety, comfort, and trust in the care they receive. Remember, protecting privacy is not just a legal requirement – it is a crucial part of providing compassionate and respectful care.
Where can you find more information

by editor | Dec 11, 2022 | Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Office Team, Hospice 101 - Social Workers, Medical Records, Patient Care, Rules and Regulations - Nurses, Rules and Regulations - Social Workers, Rules and Regulations - Volunteers
What is the purpose of hospice quality reporting?
The Affordable Care Act authorized the establishment of a Quality Reporting Program for hospices. The Hospice Quality Reporting Program (HQRP) was established in 2014. HQRP aims to ensure that the level of quality in clinical care, symptom management, and patient and family experiences is at a high level across all hospice agencies. HQRP further aims to help patients and their families make informed decisions about end-of-life care. The measures and benchmarks reported in HQRP also provide CMS with measurements of hospice agency performance and how agencies are performing relative to other agencies in their region and across the nation. Some of the measures can also be used as indicators of Medicare fraud or abuse.
The Affordable Care Act also requires that quality measures relating to hospice care are reported on a CMS website.
HQRP data collection began in 2014 with two components. The first component was related to Hospice Item Set (HIS) data collection and transmission. The second component was related to the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Hospice Survey participation.
The Hospice Compare website was launched in 2017, enabling patients and their families to compare between the performance of different hospice agencies. In December 2020, Hospice Compare was replaced by Care Compare.
Which measures are included in HQRP?
HQRP measures care across a patient’s hospice stay. With a commitment to quality improvement, data transparency, and informed decision-making, the number of HQRP measures has increased since the launch of the program. As of 2022, HQRP includes four metrics, each of which includes several underlying measures:
What determines HQRP Compliance?
Performance level is not considered when determining compliance with HQRP; CMS requires a hospice agency to submit data completely, and on time, to be considered compliant. A Medicare-certified hospice agency is HQRP compliant if it submits the required data within the required timeframe and the data is accepted. A hospice agency is not compliant if it submits data but the data is not accepted. Failure to comply with HQRP requirements results in a two percentage point reduction in Annual Payment Update (APU). That is, for a hospice agency to preserve its full payment update, the agency must meet all HQRP data submission requirements. Failure to submit results will also impact an agency’s results on Care Compare.
How does CMS use the data that is submitted?
CMS currently uses the collected data internally for strategic planning purposes. CMS also uses the act of reporting to raise attention and awareness and promote actions to improve patient care.
Can a hospice agency verify its HQRP data before it is publicly published?
A hospice agency can review its HQRP data via the CASPER system before the results are made public on Care Compare. CASPER reports can be accessed by selecting the CASPER Reporting link to the CMS Quality Improvement and Evaluation System (QIES) Systems for Providers webpage. Hospice-specific reports are located in the Hospice Provider and Hospice Quality Reporting Program reporting categories in CASPER. Hospice agencies should review this data before it is published on Care Compare to ensure data accuracy, since the published data is used by the public to compare and select a hospice agency for end-of-life care.
Where can you find more information?

by editor | Oct 21, 2022 | Compliance and Regulatory - Directors, Recruitment and Retention, Rules and Regulations - Nurses
What is a hospice volunteer?
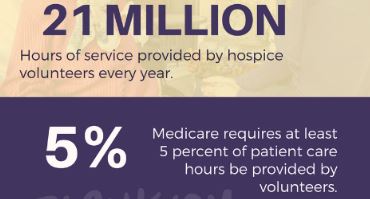
Hospice volunteers are key contributors to a hospice agency. The hospice movement was started with volunteers and there are now more than 460,000 volunteers nationwide. To retain the initial spirit of hospice, Medicare requires that volunteers must provide services that equal at least 5% of the total patient care hours of all paid hospice employees and contract staff. Hospice volunteers are used to perform day-to-day administrative tasks for the hospice agency or in direct patient care roles.
Where can you recruit to find volunteers?
How should a hospice screen potential volunteers?
There are a number of areas the hospice agency should consider when screening potential hospice volunteer’s:
- What is motivating the potential volunteer?
- What skills does the potential volunteer have?
- How much time does the potential volunteer have available?
- Is the potential volunteer willing to complete any necessary training?
- What is the potential volunteer’s degree of comfort with concepts surrounding death and dying including death, loss, grief, and bereavement. Does the potential volunteer have a healthy adjustment to significant loss?
- Does the potential volunteer have a capacity for empathy and sensitivity?
Considerations for retaining volunteers
If your agency has a wonderful team of volunteers, you want to be sure not to lose this group. How can you increase the chance of retention? Just like employees, retaining volunteers takes effort! Here are some tips for increasing the chance of retaining your volunteers:
- Hospice volunteers need to believe in the hospice mission.
- They should see an opportunity for personal or professional growth
- Volunteers should feel needed and feel that they are contributing – the the agency or to the patients that they care for
- Volunteers should feel supported by the hospice agency staff
- Volunteers should be able to share the emotional events that they may experience while they volunteer
by editor | Oct 20, 2022 | Compliance and Regulatory - Directors, Reports
What are hospice volunteers?
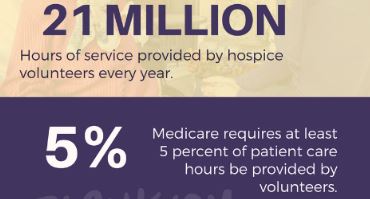
The hospice movement was started by volunteers and there are currently more than 460,000 hospice volunteers nationwide.
To retain the volunteer-based essence of hospice, one of the Medicare conditions of participation requires that hospices incorporate volunteer services into their daily patient care and operations routine.
Is there a requirement on the number of hospice volunteer hours?
Medicare requires that volunteer must provide services that equal at least 5% of the total patient care hours of all paid hospice employees and contract staff. Read more about this requirement here: What is a hospice’s volunteer requirement?
How is the Medicare 5% requirement calculated?
The percentage of volunteer time is calculated in three steps:
- Step 1: Calculate the sum of volunteer direct care patient hours plus volunteer bereavement support patient hours plus volunteer administrative hours. See What is a hospice’s volunteer requirement? for clarification on these various types of volunteer hours and activities as well as clarification on what volunteer activities may be applied for use in this calculation.
- Step 2: Calculate the sum of employee direct care patient hours plus contractor direct care patient hours
- Step 3: Divide the number in Step 1 by the number in Step 2 and multiply by 100. The result is the percentage of volunteer hours
What activities performed by hospice employees or contractors are included?
Similar to the limitations placed on volunteer activities that may be included for the purposed of this Medicare match calculation, not all activities performed by a hospice’s employees or contractors are included in Step 2.
Hours for the following staff are included in the calculation (though others may be included as well): nurse, social worker, physician, physical therapist, hospice aide, chaplain, bereavement counselor
- All direct care activities are included in the calculation
- Telephone calls to patients, families, or surviving family members are included
- Staff education time is not included
- IDG time is not included
Where can you get more information?
Read more about hospice volunteer requirements: NHPCO Hospice Volunteer FAQ

by editor | Oct 20, 2022 | Compliance and Regulatory - Directors, Reports, Rules and Regulations - Nurses
Volunteers are an essential components of hospice. The hospice movement was started by volunteers. There are currently more than 460,000 hospice volunteers nationwide. Volunteers provide administrative support or direct patient care services.
Are hospices required to have volunteers?
Use of volunteers is a Medicare condition of participation. Medicare requires the use of hospice volunteers for any Medicare certified hospice. Volunteers must be used in day to day administrative tasks that support direct patient care activities and/or in direct patient care roles.
For each hospice agency, volunteer hours must equal 5% of total patient care hours for all paid hospice agency employees and contractors. A hospice must maintain records of the number of hours worked by volunteers as well as the types of activities performed and whether these activities were administrative or patient care.
The hospice volunteers must perform their activities under the supervision of a designated hospice employee.
Are there other volunteer-related requirements?
There are additional training and documentation requirements that a hospice agency must meet, relating to hospice volunteers:
- A hospice must provide orientation and training for its hospice volunteers and this training must documented
- Efforts to recruit volunteers on an ongoing basis must be documented
- Cost savings achieved through the use of volunteers must be documented. The documentation must include the volunteer’s position, the time spent by the volunteer, and the estimated dollars that would have been spent by the hospice had this position been filled by a paid hospice employee
What direct patient care activites are performed by a volunteer?
Volunteers travel to the location where the patient currently resides – such as the patient’s home, a nursing home, or an assisted living facility – and work directly with patients, caregivers, and families. These volunteers are considered direct care volunteers. Examples of direct care activities include:
- Performing light household chores
- Cooking meals
- Provide transportation for patients or their families
- Provide companionship to the patient
- Providing respite so that family caregivers can take a break
- Using some special skills that the volunteer has such as giving a manicure, giving a haircut, playing a musical instrument, doing an art project with the patient, and the like
- Travel time to the patient’s home may also be included in volunteer hours, if travel time is also used in the calculation of hospice employee hours
- Time a volunteer
What indirect care activities are performed by a volunteer?
Volunteers can also have an impact without directly interacting with patients. For example, they can prepare items that are delivered to patients, they can advocate for hospice patients in the community, or they can go to volunteer health fairs. Indirect care hospice volunteers can also assist the hospice agency with administrative and general office tasks. Examples of indirect care activities include:
- Assisting with preparing mailings for community outreach
- Assisting with data entry, filing, copying, or other clerical duties
- Answering phone calls,
- Preparing blankets to be delivered to hospice patients
- Helping setup for community events
- Helping with grief support groups
What activities may be included in the calculation of volunteer time?
There activities that may be included in total hospice volunteer hours are varied. For example:
- Time that the volunteer is performing the actual tasks (such as assisting with mailings, data entry, light housekeeping, etc.)
- Telephone calls to hospice patients, their family members, caregivers, or bereaved family members
- Travel time to patient homes, if this travel time is included in the calculation of hours for hospice employees
- Time spent receiving orientation to a specific patient
- Time spent in training to perform specific tasks
What activities may not be included in the calculation of volunteer time?
Recall that volunteers must be used in day to day administrative and or direct care patient roles. So the following are examples of activities that would not be included in the calculation of total volunteer hours:
- Flower arranging
- Working in a thrift shop
- General volunteer training that is not specific to a patient or to an administrative task
- Participation in the agency’s governing board
Where can you find out more?
by editor | Sep 15, 2022 | Accounts Payable, Billing, Billing - General, Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Office Team, Hospice 101 - Social Workers, Human Resources, Intake, Medical Records, Metrics and KPIs, Office Setup, Payroll, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Social Workers, Rules and Regulations - Volunteers
Are you confused by the Acronym Alphabet Soup?
Does the never ending list of acronyms used in the hospice and healthcare industry leave you confused?
Are you worried that you may confuse CMN with CMP?
To help sort out the confusion, we add here links to lists of acronyms:
Use these acronym listings to help clarify things when you inevitably are faced with acronym confusion!