Hospice Acronym Alphabet Soup
Are you confused by the Acronym Alphabet Soup?
Does the never ending list of acronyms used in the hospice and healthcare industry leave you confused?
Are you worried that you may confuse CMN with CMP?
To help sort out the confusion, we add here links to lists of acronyms:
- Acronyms commonly found on the cms.hhs.gov website as well as other acronyms commonly used in hospice and healthcare: Acronyms – from CMS
- A hospice quality reporting acronym list: Acronyms – from HQRP
- NHPCO acronym listing: NHPCO acronyms
Use these acronym listings to help clarify things when you inevitably are faced with acronym confusion!

Timely filing of Notice of Election
A hospice must file a Notice of Election (NOE) within five days after the beneficiary’s hospice admission date.
What is considered timely filing of an NOE?
For an NOE to be considered timely:
- The NOE must have a receipt date within five calendar days after the hospice admission date
- The NOE must process and finalize in status/location P B9997
For example:
- Patient admitted on 5/8
- NOE submitted on 5/13
- NOE processed on 5/27
To be timely, the NOE must have a receipt date of 5/13 and the NOE must subsequently process (P B9997)
However, if the NOE is not filed timely, Medicare will not cover and pay for the days of hospice care from the date that the patient is admitted until the date the NOE is submitted and accepted. For example:
- Admission date: 5/1
- NOE receipt date 5/10
- NOE processed 5/18
Non covered days: 5/1 through 5/9 (one day before NOE receipt date)
- Admission date 5/1
- NOE receipt date 5/10
- NOE processed 5/18
Non covered days: 5/1 through 5/9 (one day before NOE receipt date)
What happens if a hospice must resubmit an NOE due to errors?
Sometimes an NOE is submitted but it is not accepted due to a need for corrections. The NOE is “RTPd” (Returned to Provider) and is then resubmitted by the hospice. The date that the NOE is resubmitted by the hospice is considered the submission date.
How should a hospice file a claim if the NOE was filed late?
If a hospice has a late NOE, the claim must be filed showing the late filed NOE. It must also show occurrence code OSC 77, indicating the non covered dates. The claim will have two rows, one row for the non-covered days and one row for the covered days.
See Submitting Claims for Untimely NOEs for more details on billing when NOEs are untimely.
For more information on submitting claims, read some of our posts here Hospice Keys Billing Blogs
What is a MAC?
A Medicare Administrative Contractor (MAC) is a private health care insurer that has been awarded a geographic jurisdiction to process Medicare Part A and Part B medical claims for Fee For Service (FFS) beneficiaries.
CMS relies on these contractors to serve as the primary operational contact between the Medicare FFS program and the health providers enrolled in the program.
MACs are multi-state regional contractors who are responsible for administering Part A and Part B claims.
What types of MACs are there?
There are two types of MACs: Part A/B MACs and DME MACs.
Hospice claims are administered by Part A/B MACs. Part A/B MACs process about 95% of all FFS claims.
There are 12 Part A/B MACs.
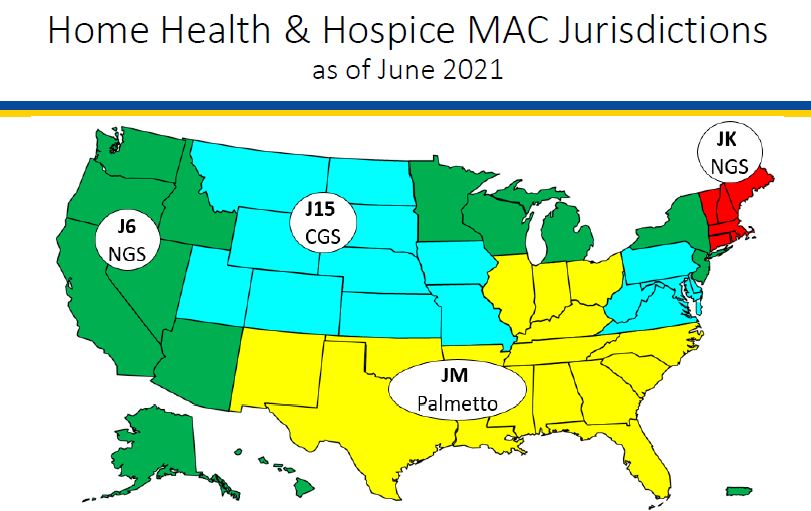
Four of the MACs specialize in processing claims for hospice and home health providers
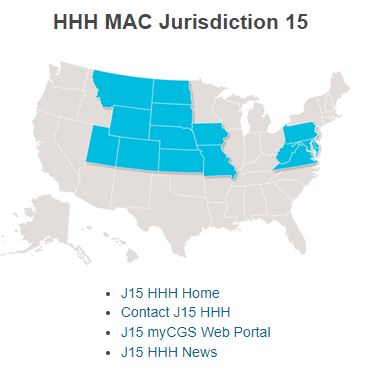
What geographic areas do each of the hospice and home health MACs cover?
The following map shows the geographic regions that each of the hospice MACs is responsible for administering.
What activities do MACs perform?
MACS perform a number of activities including:
- Provider Enrollment
- Claims processing, payment, and payment notices
- Provider customer service (but not beneficiary customer service)
- Audit provider cost reports
- Respond to provider inquiries
- Audit payments and review medical records
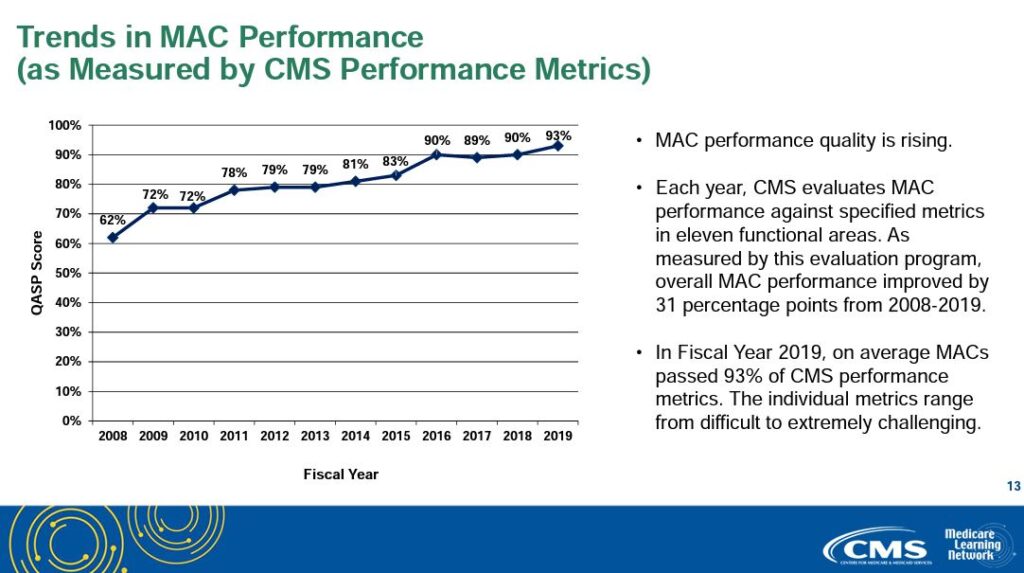
How are MACs measured and how well do they perform?
Each year, CMS evaluates MAC performance against specific metrics in eleven functional areas. MAC performance quality has been consistently improving since CMS began measuring MAC performance. Average MAC performance has increased from 62% to 93% since CMS began measuring MAC performance.
Print ‘n take hospice keys
- Seeking to contact your MAC? Here’s their contact information
- A map of MAC regional jurisdictions
Where can you find more information?
This PowerPoint from Medicare Learning Network provides more helpful information about MACs: MLN MAC PowerPoint
How to Submit a Notice of Election
What is a Notice of Election?
When a Medicare beneficiary elects hospice services, the hospice must complete an election notice with the beneficiary and file a Notice of Election (NOE) with Medicare.
When must a Notice of Election be submitted?
A hospice notice of election must be submitted and processed prior to submitting the first hospice claim. Beginning October 1, 2014, Medicare has implemented a requirement that the hospice agency must file a NOE within 5 calendar days after the date of the hospice election notice.
In addition to filing the NOE, the NOE must be accepted by the Medicare claims system. For an NOE to be accepted, it must be a “clean submission.” That is, the NOE may not have any errors.
If the NOE has any errors, it will be returned to the provider (RTP’d) for correction. When the provider corrects and resubmits the NOE, the NOE will be assigned a new received date. This new date will be used to establish timely filing with respect to Medicare’s five day requirement.
There are three ways that a hospice provider can submit an NOE
– Using Direct Data Entry (DDE):
DDE is a real time Fiscal Intermedicary Shared System (FISS) application that gives hospice providers the ability to submit claims, monitor the status of claims, and correct claims. It can also be used by providers to monitor claims and requested documentation and to check beneficiary eligibility information.
Providers can manually enter the NOE into DDE via the different relevant screens.
– Submit electronically:
This option became available effective January 1, 2018. The hospice industry requested requested that Medicare implement NOE submission via Electronic Data Exchange (EDI), as this would eliminate keying errors associated with NOE (and thus reduce the number of NOEs that were RTP’d for keying errors since the data for the NOE could be exported directly from the patient’s electronic medical record). Note that NOEs should not be batched with claims
– Paper submission on UB-04 claim forms. .
Where can you find detailed information about completing the NOE?
A helpful job aid has been created that provides details on how to complete the notice of election, with details on the different data requirements depending upon the method of submission: Palmetto NOE job aid

Unusual Circumstances: Face to Face Encounters
Prior to the third hospice benefit period, and prior to each subsequent benefit period, a hospice physician or nurse practitioner is required to have a face to face encounter with the hospice patient to recertify that the patient continues to be Medicare eligible for hospice benefits. The face to face encounter must occur within 30 calendar days prior to the start of the third benefit period and each subsequent benefit period.
The face to face encounter is necessary to recertify that the patient remains eligible for Medicare hospice benefits. If face to face encounters are not performed timely, the patient is is no longer hospice eligible. The hospice may continue to provide hospice services to the patient but may no longer continue to bill Medicare. Instead, the hospice would need to assume all financial responsibility for the patient until such time that the hospice is able to reestablish patient hospice eligibility. The patient may be readmitted to hospice once hospice eligibility criteria are once again met.
What if there are exceptional circumstances that cause the hospice to be unable to timely complete the face to face encounter?
What are exceptional circumstances?
If a patient is admitted and is in the third benefit period or later, the hospice agency may be unable to perform the face to face encounter prior to the start of the benefit period.
For example, if the patient is an emergency weekend admission and the nurse practitioner or hospice physician is unable to meet with the patient prior to hospice admission. The patient is only seen the following Monday.
Another exceptional circumstance may be where the CMS data system is unavailable and the hospice agency is unaware that the patient is in the third or later benefit period.
In these documented exceptional circumstances, the face to face encounter is considered timely if it is completed within two days after admission.
In addition, if the patient dies within two days of admission, the face to face encounter is considered complete.
Where can you get more information?
Details on Medicare Face to Face encounter requirements: Medicare F2F encounter requirements
