by editor | Nov 13, 2022 | Compliance and Regulatory - Directors, Documentation - Chaplains, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Intake, Medical Records, Metrics and KPIs, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Office Team, Rules and Regulations - Social Workers
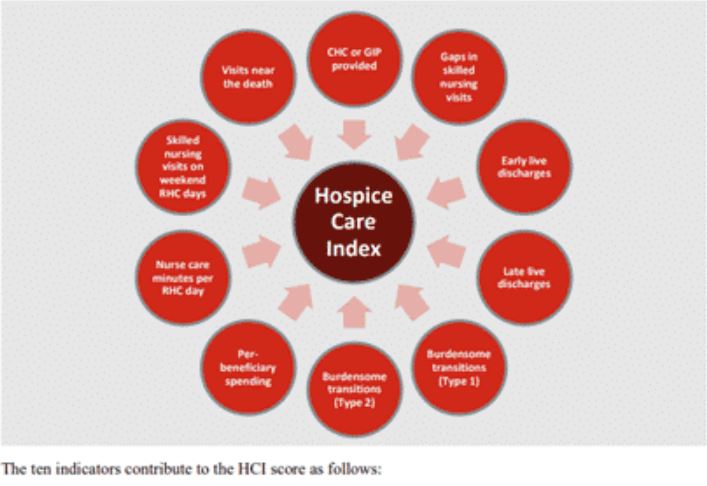
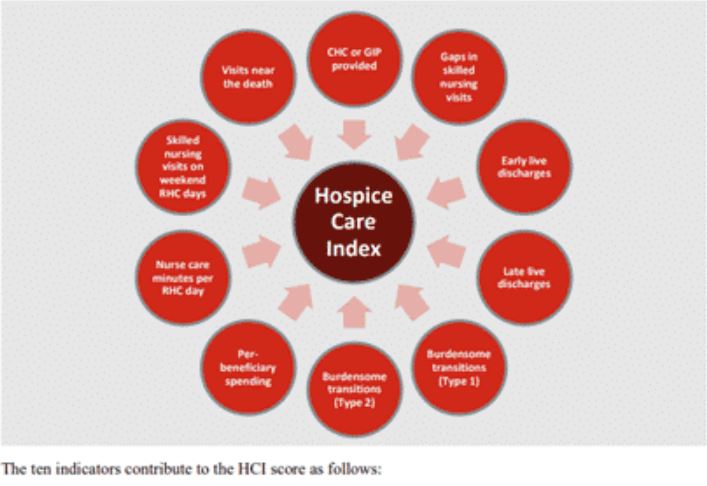
HCI is a single comprehensive metric reflecting ten indicators of care delivered during a hospice stay — from admission to discharge. This metric, which is included in the patient Care Compare portal, is intended to provide patients, families, and caregivers with an added metric to support informed healthcare choices.
What are the data sources for this metric?
HCI is calculated from Medicare claims data. A hospice agency does not need to submit any additional data to CMS for the calculation of this metric. The HCI metric captures care processes throughout the duration of a patient’s hospice care – from admission through discharge. Only data for Medicare fee for service patients who have been discharged from hospice is included in the HCI metric. CMS calculates HCI using eight consecutive quarters of data. Hospice agencies with fewer than 20 discharges in the reporting period are not assigned an HCI value. By including eight quarters of data, CMS is expanding the set of hospice agencies for which an HCI value will be reported. CMS will update the HCI metrics once each year.
What does the HCI metric measure?
HCI is a single comprehensive metric comprised of the following ten individual indicators of care.
- CHC/GIP provided
- Gaps in skilled nursing visits
- Early live discharges
- Late live discharges
- Burdensome transitions (Type 1)
- Burdensome Transitions (Type 2)
- Per-beneficiary Medicare spending
- Nurse care minutes per routine home care days
- Skilled nursing minutes on weekends
- Visits near death
Each indicator measures a different aspect of hospice care. A set of the HCI indicators measure the agency’s provision of higher level of care as needed and more frequent visits closer to the time of death, as measured by indicators
- Gaps in skilled nursing visits
- Nurse care minutes per routine home care day
- Skilled nursing minutes on weekends
- Visits near death
A set of HCI indicators measure patterns of live discharges and transitions, as measured by indicators
- Discharges from hospice followed by hospitalization and hospice readmission
- Discharge from hospice followed by patient dying in the hospital
- Early live discharges
- Late live discharges
Finally, an HCI indicator is used to measure appropriateness of use of the hospice benefit
- Per beneficiary Medicare spending
Medicare’s overall objectives of the HCI metric are twofold: (i) to ensure that all hospice patients are receiving the care that they need and (ii) to identify indicators of fraud.
How is the HCI metric calculated?
The HCI metric simultaneously monitors all ten indicators of care. The ten indicators are then combined into a single value between zero and ten, where ten is the highest value. Each indicator equally affects the HCI value, reflecting how each aspect of care delivered, from admission to discharge, shares the same level of importance.
Specifically, the hospice agency is awarded one point for each of the ten indicator criteria the agency meets. A hospice receives a point for an indicator if its value exceeds a prescribed threshold. The threshold is determined as a function of the overall values for that indicator across all hospice agencies. The more indicators a hospice agency meets, the higher the agency’s HCI value. The sum of the points earned from meeting the criterion for each indicator yields the agency’s aggregated single HCI value.
When was HCI introduced and where can the metric be viewed?
The HCI metric was added to the HQRP and began public reporting in 2022.
The single aggregate HCI metric can be seen under the Quality of Patient Care section on the Care Compare website.
The details of the HCI metric – including the values for each of the ten individual HCI indicators – can be found in the Provider Data Catalog.
How can a hospice see details about its HCI value?
To support a hospice agency’s quality improvement efforts, CMS shares the details of an agency’s HCI indicator scores in the Hospice Agency Level QM Report in CASPER. An agency can benchmark its indicator values with state and national averages. It can also trend its performance in each indicator over time.
Where can you learn more?
Image from Home Care Pulse
by editor | Oct 18, 2022 | Billing, Billing - General, Compliance and Regulatory - Directors, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Office Team, Hospice 101 - Social Workers, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Social Workers
To receive hospice services under the Medicare benefit, a patient or his authorized representative must elect hospice care.
If the patient or authorized representative elects to receive hospice care, the patient must file an election statement with a specific hospice agency. The election statement serves to indicate that the patient is choosing hospice care.
The election statement and the election statement addendum are conditions for payment.
What is the structure of a hospice election form?
Every hospice agency can design and create their own hospice election statement form although Medicare has published a model form that can be used by hospice agencies Model Hospice Election Statement. The election statement must include all of the following elements:
- Name of hospice agency that will be providing the services
- Acknowledge that nature of hospice services have been explained to the patient including, in particular, the palliative rather than curative nature of care
- Acknowledge patient understands that by electing hospice care, some Medicare services are waived
- For hospice elections beginning on or after October 1, 2020, a statement that although it would be rare, there could be some necessary items, drugs, or services that may not be covered by hospice because these items are deemed to be unrelated to the terminal illness or related conditions
- The effective date of the election. This may be the first day of hospice care of a later day. But it cannot be a date that precedes the date that the election statement was signed by the patient or their authorized representative.
- The individual who is serving as the patient’s attending physician, if any.
- Acknowledgement that the identified attending physician was the choice of the patient or authorized representative
- Signature of patient or authorized representative
There are some additional requirements for the election statements for elections beginning dated October 1, 2020 or later. These election statements must also include :
- Information on patient cost sharing for hospice services
- Notification of the patient or authorized representative right to receive an addendum to the election statement. The addendum is only required to be furnished to beneficiaries, their authorized representatives, non-hospice providers, or Medicare contractors who request this information. This addendum includes a list and rationale for the items, drugs, or services that are not covered by hospice services because the hospice has deemed these to be unrelated to the terminal illness and related conditions.
- Information on the Beneficiary and Family Centered Care Quality Improvement Organization (Beneficiary and Family Centered Care (BFCC) ), including that immediate advocacy is available through this organization if the patient disagrees with the hospice’s determination regarding non-covered services
Right to Request Patient Notification of Non-Covered Items, Services, And Drugs
At any time, a patient may request, in writing, the Patient Notification of Hospice Non-Covered Items, Services, and Drugs. addendum to the election statement.
The hospice agency must provide the notification within five days, if this request is made on the start of care date.
If the request is made during the course of hospice care, the hospice agency must provide the requested notification within 72 hours.
If the patient (or authorized representative) requests the addendum at the start of care but dies with five days, the hospice is deemed to have met its requirement and is not required to provide the addendum.
When would a hospice update the addendum?
The addendum lists the patient’s diagnoses and conditions that are present upon hospice admission and the items, services, and drugs that are not covered by the hospice because they are deemed to be unrelated to the terminal illness and related conditions.
During the course of hospice care, the addendum may require update, for example, if the patient’s plan of care is updated.
Changes to the addendum will need to be signed by the patient or his authorized representative and stored in the patient’s medical record with the hospice agency.
Where can you find more information on the election statement
by editor | Sep 15, 2022 | Accounts Payable, Billing, Billing - General, Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Office Team, Hospice 101 - Social Workers, Human Resources, Intake, Medical Records, Metrics and KPIs, Office Setup, Payroll, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Social Workers, Rules and Regulations - Volunteers
Are you confused by the Acronym Alphabet Soup?
Does the never ending list of acronyms used in the hospice and healthcare industry leave you confused?
Are you worried that you may confuse CMN with CMP?
To help sort out the confusion, we add here links to lists of acronyms:
Use these acronym listings to help clarify things when you inevitably are faced with acronym confusion!


by editor | Aug 4, 2022 | Billing, Billing - General, Compliance and Regulatory - Directors, Documentation - Nurses, Financials, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Office Team, Intake, Patient Care, Patient Eligibility, Rules and Regulations - Nurses, Rules and Regulations - Office Team
A hospice face to face encounter is a step in patient recertification beginning with the third benefit period and each benefit period thereafter. The goal of hospice face to face patient encounter is to encourage greater involvement of the physician in the care of patients who have been on hospice for an extended period of time. These patients will require a face to face visit from the physician or from a hospice nurse practitioner who will determine continued hospice eligibility. The face to face encounter is one part of hospice recertification. As such, the face to face encounter will also occur prior to recertification.
When must a face to face encounter take place?
A face to face encounter must take place within 30 days prior to the start of the patient’s third benefit period. It also must take place within 30 days prior to each subsequent benefit period. The requirement for a face to face encounter considers the patient’s hospice stays across all hospices. For example, if a patient spent 100 days at Hospice Agency A and then switched to Hospice Agency B, Hospice Agency B will need to conduct a face to face encounter within 50-80 days of the patient’s admission. That is, when the patient is admitted to hospice B the days of counting toward the face to face encounter begin from the first day that the patient entered any hospice care.
How will I know if the patient has had prior hospice care?
Upon admitting a patient, the hospice agency should check the Common Working File to determine the patient benefit period and whether a face to face encounter is required.
Who may conduct the face to face encounter?
Either the hospice physician or nurse practitioner (NP) may conduct the face to face encounter. The hospice physician may be an employee or contracted by the hospice agency. If the NP conducts the face to face encounter, the NP must be an employee of the hospice and is not permitted to be a contractor (since nursing is a core service).
What should the recertification narrative include?
The third benefit recertification – and each subsequent recertification – will need to contain clinical findings that support continued hospice eligibility. The narrative must include an explanation of why the clinical findings support a life expectancy of six months or less.
If the physician conducts the face to face, he or she will be responsible to write the narrative about the clinical findings regarding the patient’s condition and for certifying the patient’s continued eligibility for hospice.
If the nurse practitioner conducts the face to face encounter, he or she will report back the clinical findings to the interdisciplinary team as well as to the hospice physician who will certify as to whether the patient is eligible for continued hospice care.
The recertification requires an attestation
The clinician who conducts the face to face encounter must attest in writing that the face to face encounter was performed with the patient and must include the date that the encounter occurred.
If an NP conducts the encounter, the NP must attest that the clinical findings were sent to the certifying physician.
The attestation is signed and dated in is included as a separate and distinct section of the recertification. The recertification also clearly notes the benefit period dates for which the recertification applies.
What happens if the face to face does not take place timely?
If the face to face does not take place, the patient is considered no longer considered terminally ill and therefore is not eligible for the Medicare hospice benefit. The patient remains ineligible until such time that the face to face encounter occurs and it is confirmed that the patient is once again hospice eligible. The patient must be discharged from the hospice but can be readmitted once the face to face encounter occurs. Medicare does permit the hospice agency to continue to provide services at the agency’s expense until the patient’s eligibility is reestablished. However, this care will be provided outside of the Medicare hospice benefit.