by editor | Nov 26, 2022 | Compliance and Regulatory - Directors, Documentation - Chaplains, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Intake, Medical Records, Metrics and KPIs, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Office Team, Rules and Regulations - Social Workers
The PEPPER report target areas focus on statistics that will identify potential for improper Medicare billing. Comparison to national, jurisdictional, and state percentiles can highlight a hospice agency’s potential need for change to its practices to guard against improper billing. Hospice agencies can leverage the information on these reports to prioritize internal audit and efforts to ensure accurate billing.
Why did CMS focus on the target areas in the PEPPER report?
- Concern: Are patients eligible and is the agency providing good quality of care?
- Target Areas: Live discharges – no longer terminally ill or patient revocation
- Discussion: A hospice may discharge a patient alive because the patient is no longer eligible, the patient revoked, the patient moved out of the service area, or for cause. The first two reasons are concerning. These reasons for live discharge may indicate that the hospice is admitting patients who are not hospice eligible. If the patient revoked it may indicate that the quality of care is lacking.
- Concern: Is a hospice agency trying to take advantage of the high routine home care rate?
- Target Area: Live discharge with length of stay between 61-179 days
- Discussion: CMS pays a higher rate for the first 60 days of routine home care; the rate of payment is lower for days 61+. High incidence of live discharge in days 61+ may indicate the hospice agency is driven by financial concerns and wants to discharge patients once the rate drops.
- Concern: Is the hospice agency admitting ineligible patients?
- Target Area: Long length of stay
- Discussion: The hospice may be admitting ineligible patients and therefore have an unusually long length of stay as compared to its peers
- Concern: Is the hospice agency targeting patients in more profitable care settings?
- Target Area: Services provided in assisted living facilities
- Discussion: An OIG study published in January 2015 found that Medicare payments for hospice care to patients in assisted living facilities increased significantly. While the diagnoses of patients in this setting typically involved less complex care, these patients remained on hospice longer and hospices received higher payments than for patients in other settings. There is therefore a need to monitor whether hospices are targeting patients in more profitable care settings including assisted living facilities, skilled nursing facilities, and nursing facilities.
- Concern: Is a hospice agency accurately reporting all diagnoses on the claim?
- Target Area: Claims with a single diagnosis code:
- Discussion: A hospice should report on the hospice claim the principle diagnosis and all diagnoses related to the terminal illness and related conditions. A hospice agency that has an unusually high number of claims with a single diagnosis may indicate that the hospice is not reporting all related diagnoses.
- Concern: Is the hospice agency meeting Medicare CoP and able to offer all four levels of care?
- Target Area: No general inpatient or continuous home care
- Discussion: Medicare Conditions of Participation require hospices to demonstrate they can provide all four levels of care: routine home care, general inpatient care, inpatient respite care, and continuous home care to be a Medicare certified hospice provider. A report published by CMS in 2014, included an analysis of 2012 hospice claims:
- 3% of beneficiaries did not have any general inpatient care in 2012
- 1% of hospice agencies did not provide any general inpatient care to any of their patients
- 4% of all hospice days billed in 2012 were billed as continuous home care
- 7% of hospice agencies billed at least one day of continuous home care but the share of continuous home care days billed varied across hospice agencies that billed any continuous home care days
- Almost 90% of hospice agencies that provided continuous home care had less than 1% of their days billed as continuous home care
- Four hospices billed more than 10% of their days as continuous home care.
This target area aims to monitor that hospice agencies are meeting the hospice Conditions of Participation and are able to provide all four levels of care.
- Concern: Is general inpatient care being used appropriately and are patient symptoms being managed well?
- Target Area: Long general inpatient stays
- Discussion: General inpatient stays are intended to be short term, to treat acute symptoms. If a patient has extended general inpatient stay there this level of care is not being used appropriately or that symptoms are not being properly managed.
- Concern: Is Medicare making prescription drug Part D payments when these should be paid by the hospice agency?
- Target Area: Medicare Part D payments for hospice beneficiaries
- Discussion: Hospice agencies are paid a per diem rate for each day that a patient is in hospice care, irrespective of the services that the hospice agency provides to the patient. Drugs that the hospice agency provides to the patient are included in the hospice rate. In 2019, CMS released a report analyzing 2016 Medicare Part D payments being made for beneficiaries on hospice care. Part D is the Medicare prescription drug plan. The study focused on four categories of drugs that are often prescribed to patients at the end of their lives as well as two disease specific drugs for two diseases. Part D should not pay for drugs if the patient is on hospice and the drug is covered under the hospice benefit. Based upon sample results, CMS estimates that Medicare paid $160.8 million for drugs that hospice agencies should have paid for, constituting and overpayment to hospice.
How can a hospice use this information?
With a better understanding of the underlying motivation for each of these target areas, a hospice agency should carefully look at the data on its PEPPER reports to identify any metrics that indicate a need for further investigation and possible process improvements. These reports are a powerful way to benchmark a hospice agency’s performance relative to itself (over a running three year period) as well as relative to other hospice agencies – across the nation, in its state, and in its MAC jurisdiction.
Where can you get more information?
by editor | Nov 13, 2022 | Compliance and Regulatory - Directors, Documentation - Chaplains, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Intake, Medical Records, Metrics and KPIs, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Office Team, Rules and Regulations - Social Workers
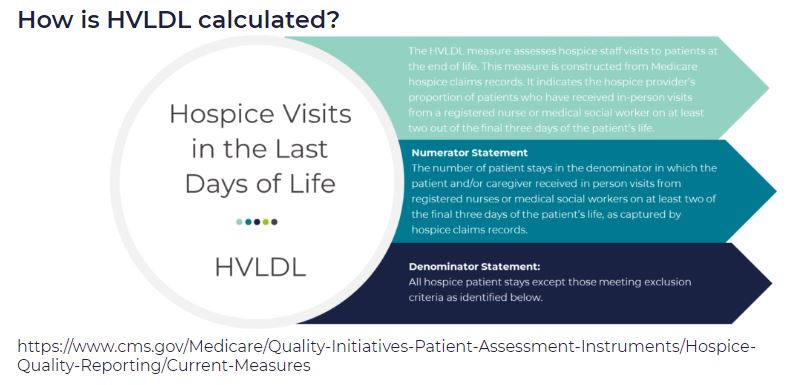
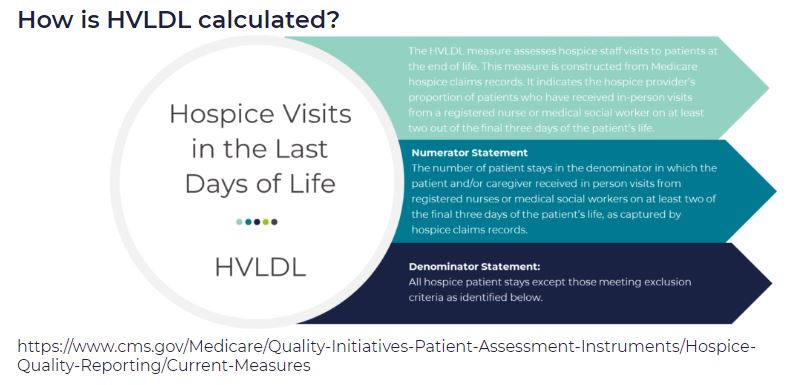
HVLDL is an HQRP claims-based measure of the proportion of patients who have received in-person visits from a registered nurse (RN) or a medical social worker (MSW) on at least two of the final three days of life. This metric replaces the HIS-based measure Hospice Visits When Death is Imminent (HVWDII).
CMS selected this metric as an important measure of quality since it is during these final days that patients most likely exhibit extreme symptoms of actively dying. This time period is also when patients most often exhibit signs of onset of clinical signs of dying. Finally, consistent visits in the final days of life are perceived as better level of care by the patient’s family.
How are the final three days of life defined?
For the purposes of HVLDL, the final three days of life are defined as:
- Day 1: day of death
- Day 2: day prior to death
- Day 3: day two days prior to death
How are days counted?
- This metric counts days, not visits
- If an RN and a MSW each visit the patient on the same day, this counts as a single day not as two visits, since the metric counts days not visits
- Telephonic visits do not count toward this metric, only in person visits
- Visits by LPN, chaplains, or other clinical staff do not count toward this metric
Which patients are included in the calculation of HVLDL?
All Medicare fee for service hospice patients are included in this metric with the following exceptions:
- Patients who did not die in hospice care
- Patients who received continuous care, respite care, or general inpatient care in the final three days of life
- Patients who were enrolled in hospice care for fewer than three days
Since HVLDL measures visits over the final three days of life, a patient must have been enrolled in hospice for at last three days to be included in the metric.
What are the data sources for this metric?
Data for HVLDL is calculated from Medicare claims data. Only data for Medicare fee for service patients who died while in hospice and who do not meet any of the exceptions listed above are included in the HVLDL calculation.
CMS calculates HVLDL using eight consecutive quarters of data. Hospice agencies with fewer than 20 “eligible patients” in the reporting period (where an “eligible patient” is defined as a patient who has died while under hospice care and does not fall under any of the exceptions listed above) are not assigned an HVLDL value. By including eight quarters of data, CMS is expanding the set of hospice agencies for which an HVLDL value will be reported. CMS will update the HVLDL value once each year.
How is the HVLDL metric calculated?
- The denominator is the count of all “eligible patients” during the reporting period
- The numerator is the count of all “eligible patients” who received an RN or MSW visit on at least two of the three final days of life
When was HVLDL introduced and where can patients and their families view the HVLDL value?
HVLDL was added to the HQRP in 2021 and began public reporting in 2022. The metric provides insight into care provided by the hospice agency in the days immediately leading up to patient death. HVLDL can be seen under the Quality of Patient Care section on the Care Compare website.
How can a hospice see its HVLDL value?
To support a hospice agency’s quality improvement efforts, CMS shares the agency’s HVLDL value in the Hospice Agency Level QM Report in CASPER. CASPER reports separately the numerator and denominator of HVLDL as well as the hospice observed percent – the agency’s HVLDL score. CASPER also reports on the national average HVLDL score and the agency’s percentile. Percentile rank indicates what percentage of agencies nationwide had a HVLDL score that was equal to or lower than the agency’s score. A hospice agency can benchmark its HVLDL score with the national average and the percentile rank. It can also trend its performance against its own HVLDL value over time.
Why did CMS replace the HIS HVWDII?
CMS implemented HVWDII in 2017. This metric measured hospice visits by non-clinical team members including LPN, chaplain, MSW, and hospice aides during the final seven days of a patient’s life. Analyzing the data collected by this metric, CMS found that HVWDII was unable to distinguish between high quality and low quality hospice agencies (i.e., it failed the CMS validity testing criteria). Consequently, CMS sought a replacement metric. The revised metric is also aligned with the Service Intensity Add-On (SIA) payment initiative (which incentivizes visits by RN and MSW near patient’s death). HVLDL has an added benefit that it is calculated based on claims data so it does not add a reporting burden for hospice agencies.
Where can you learn more?
Image from Medalogix
by editor | Nov 13, 2022 | Compliance and Regulatory - Directors, Documentation - Chaplains, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Intake, Medical Records, Metrics and KPIs, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Office Team, Rules and Regulations - Social Workers
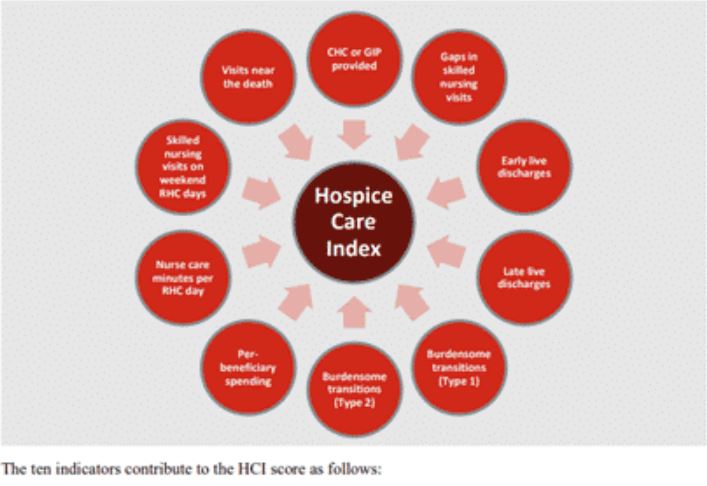
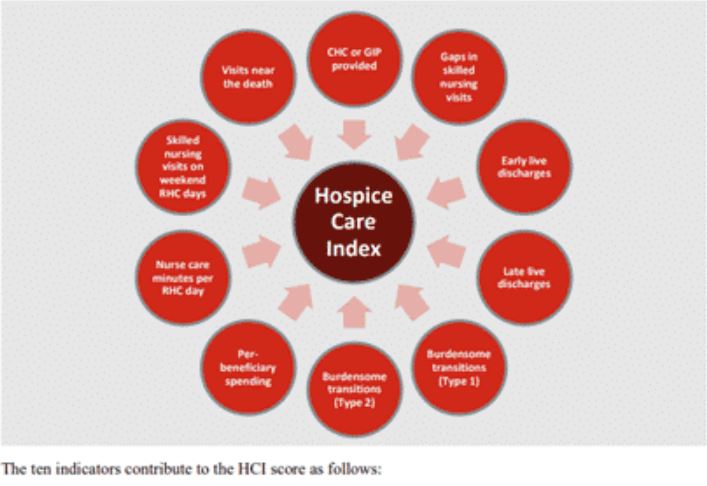
HCI is a single comprehensive metric reflecting ten indicators of care delivered during a hospice stay — from admission to discharge. This metric, which is included in the patient Care Compare portal, is intended to provide patients, families, and caregivers with an added metric to support informed healthcare choices.
What are the data sources for this metric?
HCI is calculated from Medicare claims data. A hospice agency does not need to submit any additional data to CMS for the calculation of this metric. The HCI metric captures care processes throughout the duration of a patient’s hospice care – from admission through discharge. Only data for Medicare fee for service patients who have been discharged from hospice is included in the HCI metric. CMS calculates HCI using eight consecutive quarters of data. Hospice agencies with fewer than 20 discharges in the reporting period are not assigned an HCI value. By including eight quarters of data, CMS is expanding the set of hospice agencies for which an HCI value will be reported. CMS will update the HCI metrics once each year.
What does the HCI metric measure?
HCI is a single comprehensive metric comprised of the following ten individual indicators of care.
- CHC/GIP provided
- Gaps in skilled nursing visits
- Early live discharges
- Late live discharges
- Burdensome transitions (Type 1)
- Burdensome Transitions (Type 2)
- Per-beneficiary Medicare spending
- Nurse care minutes per routine home care days
- Skilled nursing minutes on weekends
- Visits near death
Each indicator measures a different aspect of hospice care. A set of the HCI indicators measure the agency’s provision of higher level of care as needed and more frequent visits closer to the time of death, as measured by indicators
- Gaps in skilled nursing visits
- Nurse care minutes per routine home care day
- Skilled nursing minutes on weekends
- Visits near death
A set of HCI indicators measure patterns of live discharges and transitions, as measured by indicators
- Discharges from hospice followed by hospitalization and hospice readmission
- Discharge from hospice followed by patient dying in the hospital
- Early live discharges
- Late live discharges
Finally, an HCI indicator is used to measure appropriateness of use of the hospice benefit
- Per beneficiary Medicare spending
Medicare’s overall objectives of the HCI metric are twofold: (i) to ensure that all hospice patients are receiving the care that they need and (ii) to identify indicators of fraud.
How is the HCI metric calculated?
The HCI metric simultaneously monitors all ten indicators of care. The ten indicators are then combined into a single value between zero and ten, where ten is the highest value. Each indicator equally affects the HCI value, reflecting how each aspect of care delivered, from admission to discharge, shares the same level of importance.
Specifically, the hospice agency is awarded one point for each of the ten indicator criteria the agency meets. A hospice receives a point for an indicator if its value exceeds a prescribed threshold. The threshold is determined as a function of the overall values for that indicator across all hospice agencies. The more indicators a hospice agency meets, the higher the agency’s HCI value. The sum of the points earned from meeting the criterion for each indicator yields the agency’s aggregated single HCI value.
When was HCI introduced and where can the metric be viewed?
The HCI metric was added to the HQRP and began public reporting in 2022.
The single aggregate HCI metric can be seen under the Quality of Patient Care section on the Care Compare website.
The details of the HCI metric – including the values for each of the ten individual HCI indicators – can be found in the Provider Data Catalog.
How can a hospice see details about its HCI value?
To support a hospice agency’s quality improvement efforts, CMS shares the details of an agency’s HCI indicator scores in the Hospice Agency Level QM Report in CASPER. An agency can benchmark its indicator values with state and national averages. It can also trend its performance in each indicator over time.
Where can you learn more?
Image from Home Care Pulse
by editor | Sep 29, 2022 | Billing, Billing - General, Compliance and Regulatory - Directors, Financials, Rules and Regulations - Office Team
What is Medicare credit balance?
A Medicare credit balance represents a Medicare overpayment to a provider due to patient billing error or claims processing error that must be refunded to Medicare. The report is referred to as a Credit Balance Report because when a provider receives excess payment for a claim that was submitted, this is typically reflected in the provider’s accounting records (i.e., in the patient account receivable) as a “credit.”
What instances may give rise to a credit balance?
Different situations may give rise to a Medicare overpayment. For example:
- Paid twice by Medicare or may be paid by Medicare and by another insurer for the same service
- Incorrect calculation of patient deductible or patient coinsurance amount
- Paid for non-covered services
- Billed at incorrect daily rate
Which hospice agencies must file a Credit Balance Report?
If a hospice provider has more than one provider number, a separate report must be submitted for each provider number. Providers who have a low utilization (i.e., determined by the intermediary that they should file a low utilization Medicare cost report) or who file less than 25 Medicare claims per year are not required to file a Medicare Credit Balance Report.
What does a credit Balance Report Consist of?
The Credit Balance Report consists of two pages. The first page is a Detail Page, where the hospice provider enters information about each credit balance, on a claim by claim basis. Once a claim has been reported on one Credit Balance Report it should not be reported again on a subsequent Credit Balance report. The second page is a Certification Page. All providers must complete the Certification Page. The Detail Page is only required if the provider has credit balances to report.
The Detail Page
On this page, the provider must include detailed information about each Medicare claim with a credit balance, explanation why the credit balance arose, and indicate whether the credit balance is being repaid with the filing of the report.
The Certification Page
The second page of the Credit Balance Report is a certification page. Facilities that do not have any credit balances in a quarter are only required to submit the signed certification page. There are key areas of this page.
- The first area serves as a reminder that there is a requirement to file a Credit Balance Report and failure to file this report will result in suspension of Medicare payments. Further, any misrepresentations may lead to fines and further penalties
- The second area requires an officer or administrator of the hospice agency to sign a certification that that Credit Balance Report is true and accurate
- The third area requires a selection from one of three choices: (i) provider qualifies as Low Utilization Provider (ii) Detail Page included with Report (iii) no credit balances to report
When is the report due?
A hospice provider must assess any Medicare credit balances on a quarterly basis and must report any identified Medicare credit balances within 30 days of the end of each calendar quarter. The Medicare Credit Balance Report due dates are as follows:
| Quarter Ending |
Due Date |
| March 31 |
April 30 |
| June 30 |
July 30 |
| September 30 |
October 30 |
| December 31 |
January 30 |
What happens if a provider fails to submit a Credit Balance Report?
Failure to submit a Credit Balance Report by the 15th calendar day after the report due date will result in a Suspension Warning letter. If the completed report is not received within 15 calendar days from issuance of the letter, Medicare payments to the provider are suspended under a completed letter is received, accepted, and processed.
Where can you find a Credit Balance Report form?
The Credit Balance Report that must be completed and submitted is Form CMS-838, which can be found here: Medicare Credit Balance Form (pdf)
by editor | Sep 20, 2022 | Billing, Billing - General, Compliance and Regulatory - Directors, Financials, Intake, Notice of Election, Rules and Regulations - Nurses, Rules and Regulations - Office Team
by editor | Sep 8, 2022 | Billing, Billing - General, Compliance and Regulatory - Directors, Financials, Intake, Notice of Election, Rules and Regulations - Nurses, Rules and Regulations - Office Team
What is a Notice of Election?
When a Medicare beneficiary elects hospice services, the hospice must complete an election notice with the beneficiary and file a Notice of Election (NOE) with Medicare.
When must a Notice of Election be submitted?
A hospice notice of election must be submitted and processed prior to submitting the first hospice claim. Beginning October 1, 2014, Medicare has implemented a requirement that the hospice agency must file a NOE within 5 calendar days after the date of the hospice election notice.
In addition to filing the NOE, the NOE must be accepted by the Medicare claims system. For an NOE to be accepted, it must be a “clean submission.” That is, the NOE may not have any errors.
If the NOE has any errors, it will be returned to the provider (RTP’d) for correction. When the provider corrects and resubmits the NOE, the NOE will be assigned a new received date. This new date will be used to establish timely filing with respect to Medicare’s five day requirement.
There are three ways that a hospice provider can submit an NOE
– Using Direct Data Entry (DDE):
DDE is a real time Fiscal Intermedicary Shared System (FISS) application that gives hospice providers the ability to submit claims, monitor the status of claims, and correct claims. It can also be used by providers to monitor claims and requested documentation and to check beneficiary eligibility information.
Providers can manually enter the NOE into DDE via the different relevant screens.
– Submit electronically:
This option became available effective January 1, 2018. The hospice industry requested requested that Medicare implement NOE submission via Electronic Data Exchange (EDI), as this would eliminate keying errors associated with NOE (and thus reduce the number of NOEs that were RTP’d for keying errors since the data for the NOE could be exported directly from the patient’s electronic medical record). Note that NOEs should not be batched with claims
– Paper submission on UB-04 claim forms. .
Where can you find detailed information about completing the NOE?
A helpful job aid has been created that provides details on how to complete the notice of election, with details on the different data requirements depending upon the method of submission: Palmetto NOE job aid