by editor | Nov 13, 2022 | Compliance and Regulatory - Directors, Documentation - Chaplains, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Intake, Medical Records, Metrics and KPIs, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Office Team, Rules and Regulations - Social Workers
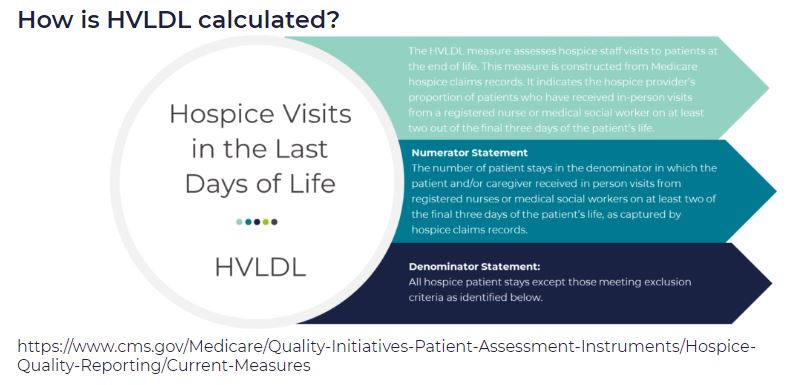
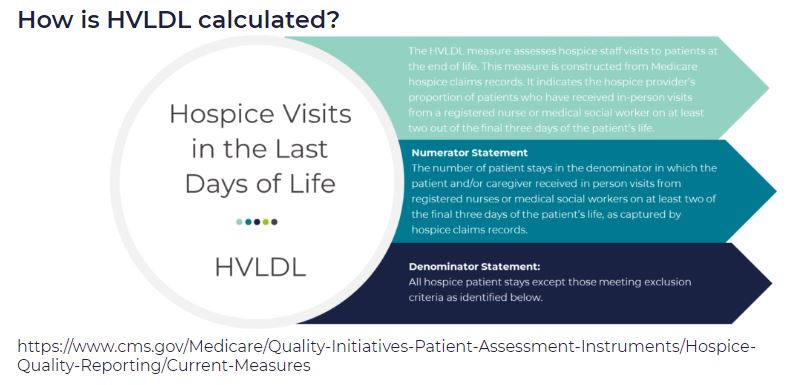
HVLDL is an HQRP claims-based measure of the proportion of patients who have received in-person visits from a registered nurse (RN) or a medical social worker (MSW) on at least two of the final three days of life. This metric replaces the HIS-based measure Hospice Visits When Death is Imminent (HVWDII).
CMS selected this metric as an important measure of quality since it is during these final days that patients most likely exhibit extreme symptoms of actively dying. This time period is also when patients most often exhibit signs of onset of clinical signs of dying. Finally, consistent visits in the final days of life are perceived as better level of care by the patient’s family.
How are the final three days of life defined?
For the purposes of HVLDL, the final three days of life are defined as:
- Day 1: day of death
- Day 2: day prior to death
- Day 3: day two days prior to death
How are days counted?
- This metric counts days, not visits
- If an RN and a MSW each visit the patient on the same day, this counts as a single day not as two visits, since the metric counts days not visits
- Telephonic visits do not count toward this metric, only in person visits
- Visits by LPN, chaplains, or other clinical staff do not count toward this metric
Which patients are included in the calculation of HVLDL?
All Medicare fee for service hospice patients are included in this metric with the following exceptions:
- Patients who did not die in hospice care
- Patients who received continuous care, respite care, or general inpatient care in the final three days of life
- Patients who were enrolled in hospice care for fewer than three days
Since HVLDL measures visits over the final three days of life, a patient must have been enrolled in hospice for at last three days to be included in the metric.
What are the data sources for this metric?
Data for HVLDL is calculated from Medicare claims data. Only data for Medicare fee for service patients who died while in hospice and who do not meet any of the exceptions listed above are included in the HVLDL calculation.
CMS calculates HVLDL using eight consecutive quarters of data. Hospice agencies with fewer than 20 “eligible patients” in the reporting period (where an “eligible patient” is defined as a patient who has died while under hospice care and does not fall under any of the exceptions listed above) are not assigned an HVLDL value. By including eight quarters of data, CMS is expanding the set of hospice agencies for which an HVLDL value will be reported. CMS will update the HVLDL value once each year.
How is the HVLDL metric calculated?
- The denominator is the count of all “eligible patients” during the reporting period
- The numerator is the count of all “eligible patients” who received an RN or MSW visit on at least two of the three final days of life
When was HVLDL introduced and where can patients and their families view the HVLDL value?
HVLDL was added to the HQRP in 2021 and began public reporting in 2022. The metric provides insight into care provided by the hospice agency in the days immediately leading up to patient death. HVLDL can be seen under the Quality of Patient Care section on the Care Compare website.
How can a hospice see its HVLDL value?
To support a hospice agency’s quality improvement efforts, CMS shares the agency’s HVLDL value in the Hospice Agency Level QM Report in CASPER. CASPER reports separately the numerator and denominator of HVLDL as well as the hospice observed percent – the agency’s HVLDL score. CASPER also reports on the national average HVLDL score and the agency’s percentile. Percentile rank indicates what percentage of agencies nationwide had a HVLDL score that was equal to or lower than the agency’s score. A hospice agency can benchmark its HVLDL score with the national average and the percentile rank. It can also trend its performance against its own HVLDL value over time.
Why did CMS replace the HIS HVWDII?
CMS implemented HVWDII in 2017. This metric measured hospice visits by non-clinical team members including LPN, chaplain, MSW, and hospice aides during the final seven days of a patient’s life. Analyzing the data collected by this metric, CMS found that HVWDII was unable to distinguish between high quality and low quality hospice agencies (i.e., it failed the CMS validity testing criteria). Consequently, CMS sought a replacement metric. The revised metric is also aligned with the Service Intensity Add-On (SIA) payment initiative (which incentivizes visits by RN and MSW near patient’s death). HVLDL has an added benefit that it is calculated based on claims data so it does not add a reporting burden for hospice agencies.
Where can you learn more?
Image from Medalogix
by editor | Nov 13, 2022 | Compliance and Regulatory - Directors, Documentation - Chaplains, Documentation - Nurses, Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Intake, Medical Records, Metrics and KPIs, Rules and Regulations - Chaplains, Rules and Regulations - Nurses, Rules and Regulations - Office Team, Rules and Regulations - Social Workers
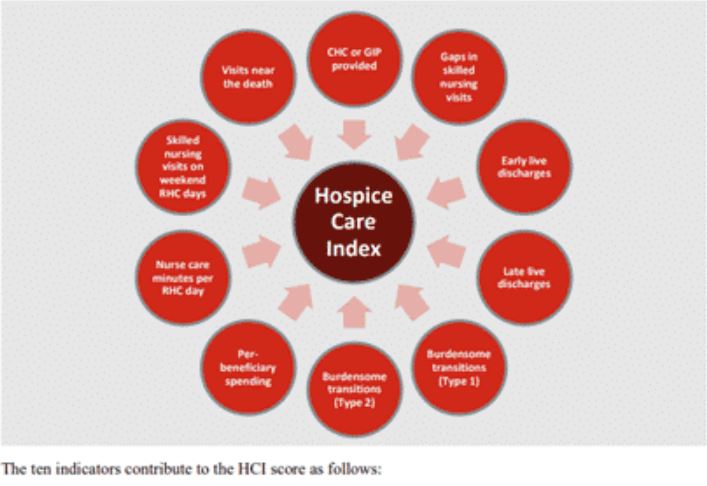
HCI is a single comprehensive metric reflecting ten indicators of care delivered during a hospice stay — from admission to discharge. This metric, which is included in the patient Care Compare portal, is intended to provide patients, families, and caregivers with an added metric to support informed healthcare choices.
What are the data sources for this metric?
HCI is calculated from Medicare claims data. A hospice agency does not need to submit any additional data to CMS for the calculation of this metric. The HCI metric captures care processes throughout the duration of a patient’s hospice care – from admission through discharge. Only data for Medicare fee for service patients who have been discharged from hospice is included in the HCI metric. CMS calculates HCI using eight consecutive quarters of data. Hospice agencies with fewer than 20 discharges in the reporting period are not assigned an HCI value. By including eight quarters of data, CMS is expanding the set of hospice agencies for which an HCI value will be reported. CMS will update the HCI metrics once each year.
What does the HCI metric measure?
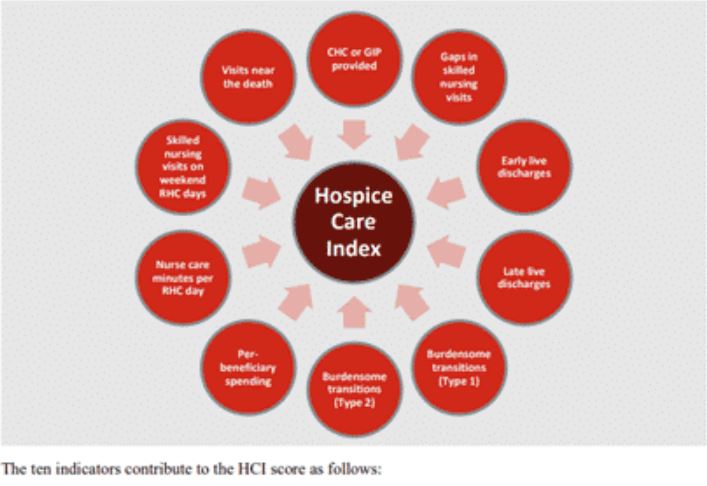
HCI is a single comprehensive metric comprised of the following ten individual indicators of care.
- CHC/GIP provided
- Gaps in skilled nursing visits
- Early live discharges
- Late live discharges
- Burdensome transitions (Type 1)
- Burdensome Transitions (Type 2)
- Per-beneficiary Medicare spending
- Nurse care minutes per routine home care days
- Skilled nursing minutes on weekends
- Visits near death
Each indicator measures a different aspect of hospice care. A set of the HCI indicators measure the agency’s provision of higher level of care as needed and more frequent visits closer to the time of death, as measured by indicators
- Gaps in skilled nursing visits
- Nurse care minutes per routine home care day
- Skilled nursing minutes on weekends
- Visits near death
A set of HCI indicators measure patterns of live discharges and transitions, as measured by indicators
- Discharges from hospice followed by hospitalization and hospice readmission
- Discharge from hospice followed by patient dying in the hospital
- Early live discharges
- Late live discharges
Finally, an HCI indicator is used to measure appropriateness of use of the hospice benefit
- Per beneficiary Medicare spending
Medicare’s overall objectives of the HCI metric are twofold: (i) to ensure that all hospice patients are receiving the care that they need and (ii) to identify indicators of fraud.
How is the HCI metric calculated?
The HCI metric simultaneously monitors all ten indicators of care. The ten indicators are then combined into a single value between zero and ten, where ten is the highest value. Each indicator equally affects the HCI value, reflecting how each aspect of care delivered, from admission to discharge, shares the same level of importance.
Specifically, the hospice agency is awarded one point for each of the ten indicator criteria the agency meets. A hospice receives a point for an indicator if its value exceeds a prescribed threshold. The threshold is determined as a function of the overall values for that indicator across all hospice agencies. The more indicators a hospice agency meets, the higher the agency’s HCI value. The sum of the points earned from meeting the criterion for each indicator yields the agency’s aggregated single HCI value.
When was HCI introduced and where can the metric be viewed?
The HCI metric was added to the HQRP and began public reporting in 2022.
The single aggregate HCI metric can be seen under the Quality of Patient Care section on the Care Compare website.
The details of the HCI metric – including the values for each of the ten individual HCI indicators – can be found in the Provider Data Catalog.
How can a hospice see details about its HCI value?
To support a hospice agency’s quality improvement efforts, CMS shares the details of an agency’s HCI indicator scores in the Hospice Agency Level QM Report in CASPER. An agency can benchmark its indicator values with state and national averages. It can also trend its performance in each indicator over time.
Where can you learn more?
Image from Home Care Pulse

by editor | Nov 7, 2022 | Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Nurses, Metrics and KPIs, Rules and Regulations - Nurses
What is the CAHPS hospice survey?
The CAHPS hospice survey is administered to eligible caregivers after a patient’s death to measure the quality of care and communication provided by the hospice. A hospice agency must participate in the CAHPS Hospice Survey to be eligible for its full annual payment update (APU). Failure to participate will result in a 2% reduction in APU. For example, compliance with the 2022 CAHPS Hospice Survey affects fiscal year 2024 APU.
Are all hospices required to administer the CAHPS hospice survey?
All Medicare certified hospice agencies should participate in the CAHPS hospice survey with two exceptions:
- Size Exemption: The exemption is based upon the number of decedents the hospice served in the prior calendar year. If the hospice served fewer than 50 survey eligible decedents or caregivers in the prior calendar year, the hospice is exempt from the CAHPS hospice survey
- Age Exemption: The exemption for age of hospice is based upon the date that the hospice received its CCN. The hospice is exempt for the remainder of the calendar year in which it receives its CCN.
CMS identifies hospices that are exempt due to age. A hospice agency is not required to file a form to request Age Exemption.
CMS does not identify hospices that are exempt for due to size. A hospice agency must apply for a Size Exemption and must apply for the Size Exemption each year that it wishes to be eligible for this exemption.
How does a hospice apply for a Size Exemption?
The hospice must complete a Participation Exemption for Size Form. The form, deadlines for submission, and details for completion can be found here.
The form requires not only a count of total patients who died while in hospice care, but certain details about these patients to determine the count of survey eligible patients and caregivers. For example, the hospice will need to submit counts of the number of patients
- who were under 18 when they died
- where there is no caregiver on record
- who died within 48 hours of final admission to hospice care
and several other categories. Care must be taken that patients are only counted in one of the categories even if they fall into multiple categories, to eliminate double counting.
What happens once a hospice submits a size exemption form?
Immediately upon submission of the form, the CAHPS Hospice Survey Project team will confirm receipt of the form. This confirmation, however, is not equivalent to Size Exemption approval. CMS will review the data to determine if the exemption is met. If CMS determines that the exemption is not met, the hospice is responsible for survey administration. Hospice agencies must accurately complete the Participation Exemption for Size Form so that they are not faced with a rejection by CMS. If the Size Exemption is not met and the hospice agency has missed administering and submitting surveys, the hospice agency will face an APU reduction.
Where can you find more information?

by editor | Nov 7, 2022 | Compliance and Regulatory - Directors, Documentation - Nurses, Hospice 101 - Nurses, Metrics and KPIs, Rules and Regulations - Nurses
Why should a hospice agency use a CAHPS Hospice Survey vendor?
A hospice agency is not permitted to administer its own CAHPS Hospice Surveys. Instead, every hospice agency is required to contract with an approved CAHPS Hospice Survey vendor. The vendor will administer the CAHPS Hospice Survey on an ongoing monthly basis and submit the data.
How can a hospice agency find an approved CAHPS Hospice Survey vendor?
CMS provides a list of approved vendors, which can be found here
Tips for selecting a survey vendor
The results of the CAHPS survey are publicly reported on Care Compare. Further, failure to submit the data timely can result in penalties from CMS. Given the significance of this survey, it is important to choose a reliable and experienced vendor that understands the hospice industry and can ensure both the quality and compliance of the data that will be submitted to CMS.
Some factors to explore when evaluating vendors include:
- Maturity of the vendor’s business and its processes. When was the business formed, number of clients, number of surveys, technologies used, operational failures, and growth in staff/changes in operations in support of growth in client base.
- Conducting the Surveys. What are survey response rates, languages supported, and mediums supported.
- Data sharing. How will patient files be shared with the vendor, does the vendor work with your EMR, is there a secure way to transmit data.
- Data Security. Has the vendor ever had a data breach, what steps are taken to ensure data protection, what steps are taken to ensure no data loss, how is data backed up, in the event of a failure how quickly will data be restored.
- Data Insights. Finally, with respect to insights, what analysis is performed on the data, what reports or dashboards does the vendor provide, does the vendor help the agency understand the results.
- Fees and Billing. Models for fees for CAHPS surveys vary by vendors. Examples may be flat price billing, fee per completed survey, fee per caregiver. Additional fees may be charged for follow ups, detailed reporting to the hospice agency, analysis shared with the agency, or access to survey data, for example.
Notifying CMS of the selected vendor
A hospice agency is required to complete a form that authorizes the CAHPS Hospice Survey vendor to collect and submit survey data to CMS. If the hospice agency does not notify CMS of this authorization, the vendor may not submit the data on behalf of the agency.
The CAHPS Hospice Survey Vendor Authorization Form is used to notify CMS of vendor authorization. The form and instructions for submission can be found here
The Vendor Authorization Form must be signed and notarized. The individual who signs the form is considered the CAHPS Hospice Survey Administrator for the hospice agency. An additional individual in the agency may be designated on the form as the primary point of contact for the survey.
Timelines
The Vendor Authorization Form must be submitted three months before data is required to be submitted.
For example, patients who die between January 2023 and March 2023 will be contacted for survey between April 2023 and June 2023. Their data will be due for submission to the CAHPS Hospice Survey Data Warehouse on August 9, 2023.
If an agency is first contracting with a vendor to begin service in January 2023, the Vendor Authorization Form would need to be submitted by May 9, 2023.
Where can you find more information?

by editor | Oct 21, 2022 | Compliance and Regulatory - Directors, Recruitment and Retention, Rules and Regulations - Nurses
What is a hospice volunteer?
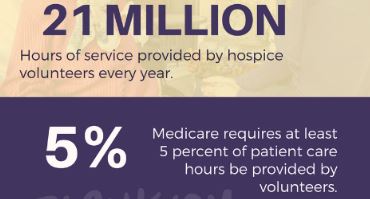
Hospice volunteers are key contributors to a hospice agency. The hospice movement was started with volunteers and there are now more than 460,000 volunteers nationwide. To retain the initial spirit of hospice, Medicare requires that volunteers must provide services that equal at least 5% of the total patient care hours of all paid hospice employees and contract staff. Hospice volunteers are used to perform day-to-day administrative tasks for the hospice agency or in direct patient care roles.
Where can you recruit to find volunteers?
How should a hospice screen potential volunteers?
There are a number of areas the hospice agency should consider when screening potential hospice volunteer’s:
- What is motivating the potential volunteer?
- What skills does the potential volunteer have?
- How much time does the potential volunteer have available?
- Is the potential volunteer willing to complete any necessary training?
- What is the potential volunteer’s degree of comfort with concepts surrounding death and dying including death, loss, grief, and bereavement. Does the potential volunteer have a healthy adjustment to significant loss?
- Does the potential volunteer have a capacity for empathy and sensitivity?
Considerations for retaining volunteers
If your agency has a wonderful team of volunteers, you want to be sure not to lose this group. How can you increase the chance of retention? Just like employees, retaining volunteers takes effort! Here are some tips for increasing the chance of retaining your volunteers:
- Hospice volunteers need to believe in the hospice mission.
- They should see an opportunity for personal or professional growth
- Volunteers should feel needed and feel that they are contributing – the the agency or to the patients that they care for
- Volunteers should feel supported by the hospice agency staff
- Volunteers should be able to share the emotional events that they may experience while they volunteer
by editor | Oct 20, 2022 | Compliance and Regulatory - Directors, Reports
What are hospice volunteers?
The hospice movement was started by volunteers and there are currently more than 460,000 hospice volunteers nationwide.
To retain the volunteer-based essence of hospice, one of the Medicare conditions of participation requires that hospices incorporate volunteer services into their daily patient care and operations routine.
Is there a requirement on the number of hospice volunteer hours?
Medicare requires that volunteer must provide services that equal at least 5% of the total patient care hours of all paid hospice employees and contract staff. Read more about this requirement here: What is a hospice’s volunteer requirement?
How is the Medicare 5% requirement calculated?
The percentage of volunteer time is calculated in three steps:
- Step 1: Calculate the sum of volunteer direct care patient hours plus volunteer bereavement support patient hours plus volunteer administrative hours. See What is a hospice’s volunteer requirement? for clarification on these various types of volunteer hours and activities as well as clarification on what volunteer activities may be applied for use in this calculation.
- Step 2: Calculate the sum of employee direct care patient hours plus contractor direct care patient hours
- Step 3: Divide the number in Step 1 by the number in Step 2 and multiply by 100. The result is the percentage of volunteer hours
What activities performed by hospice employees or contractors are included?
Similar to the limitations placed on volunteer activities that may be included for the purposed of this Medicare match calculation, not all activities performed by a hospice’s employees or contractors are included in Step 2.
Hours for the following staff are included in the calculation (though others may be included as well): nurse, social worker, physician, physical therapist, hospice aide, chaplain, bereavement counselor
- All direct care activities are included in the calculation
- Telephone calls to patients, families, or surviving family members are included
- Staff education time is not included
- IDG time is not included
Where can you get more information?
Read more about hospice volunteer requirements: NHPCO Hospice Volunteer FAQ