by editor | Aug 11, 2024 | Care Keys - Aides
Body mechanics means using your body the right way to do tasks safely and without getting hurt. When you take care of patients, it’s important to use good body mechanics to protect yourself from injuries. Let’s start by learning some key ideas that help you understand body mechanics better.
Key Concepts of Body Mechanics
- Center of Gravity
- Your center of gravity is the point in your body where your weight is balanced. For most people, this is around the belly area. Keeping your center of gravity low, like when you bend your knees, helps you stay balanced and makes it easier to lift or move things safely.
- Alignment
- Alignment means keeping your body parts in the right position. This means standing up straight, with your head, shoulders, and hips in a line. Good alignment keeps your spine straight and reduces stress on your muscles and joints.
- Base of Support
- Your base of support is the area under your feet that helps you stay balanced. When you stand with your feet apart, you have a wider base of support, which helps you stay steady, especially when lifting or moving a patient.
- Balance
- Balance is the ability to keep your body steady and not fall over. By keeping your center of gravity over your base of support, you can stay balanced. This is important when lifting or helping a patient move, so you don’t lose your balance and fall.
- Leverage
- Leverage is using your body to help lift or move something heavy. For example, when you bend your knees and lift with your legs, you’re using leverage to make the task easier. This helps protect your back from getting hurt.
Basic Rules of Body Mechanics
- Lift with Your Legs, Not Your Back
- When you lift something heavy, bend your knees and keep your back straight. Use your strong leg muscles to lift, not your back.
- Keep Objects Close to Your Body
- When you carry something, hold it close to your body. This helps keep your center of gravity low and makes it easier to stay balanced.
- Don’t Twist Your Body
- If you need to turn, move your feet instead of twisting your back or waist. Twisting can cause injuries, especially to your spine.
- Use Both Hands
- Always use both hands to lift or carry something. This helps you keep your balance and avoids putting too much strain on one side of your body.
- Push, Don’t Pull
- If you need to move something heavy, it’s safer to push it instead of pulling. Pushing uses your body weight and keeps your center of gravity over your base of support.
- Maintain a Good Posture
- Stand up straight with your shoulders back. Good posture keeps your spine in the right alignment and reduces stress on your body.
- Get Help if Needed
- If something is too heavy or awkward to move by yourself, ask for help. It’s better to be safe and avoid injury.
How to Use Proper Body Mechanics When Helping Patients
- Position Yourself Close to the Patient
- Stand close to the patient when helping them move. This gives you better control and makes the task easier by keeping your center of gravity closer to the patient’s.
- Spread Your Feet
- When lifting something heavy, spread your feet apart to create a wide base of support. This helps you stay balanced and steady while lifting.
- Bend Your Knees When Lifting a Patient
- When lifting or turning a patient, always bend your knees and keep your back straight. Use your legs for strength, and keep your body aligned to avoid injury.
- Don’t Twist Your Body
- If you need to turn while lifting a patient, move your feet instead of twisting your back or waist. Twisting can cause injuries, especially to your spine.
- Use Transfer Devices When Available
- If there’s a transfer belt, slide board, or lift device, use it to help move the patient. These tools help you use leverage and maintain good body mechanics.
- Communicate with the Patient
- Let the patient know what you’re going to do before you start. This helps them prepare and makes the move smoother, keeping both of you safe.
- Move Slowly and Carefully
- Take your time when lifting or moving a patient. Slow, controlled movements keep you balanced and prevent injuries.
Why Practicing Good Body Mechanics is Important
- Long-Term Health: Protecting your body now helps you stay healthy and pain-free for years to come.
- Job Performance: Using good body mechanics helps you do your job better and more efficiently.
- Patient Trust: When patients see you moving confidently and safely, they trust you more and feel safer in your care.
Where Can You Find More Information
by editor | Aug 11, 2024 | Care Keys - Aides, Clinical Compliance
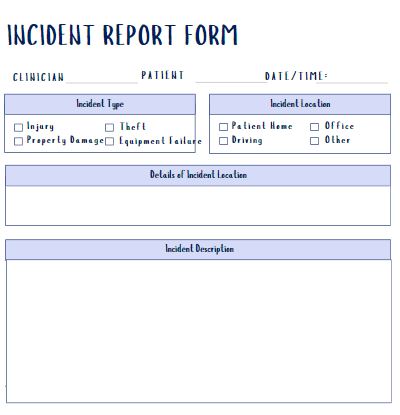
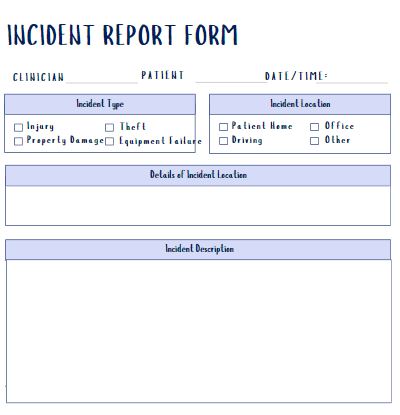
An incident report is a special kind of report that you write when something unusual or unexpected happens during your visit with a patient. This could be anything that isn’t part of the normal care routine.
When to Write an Incident Report
An incident report is needed if:
- The Patient Falls: If the patient slips, trips, or falls, even if they don’t seem hurt.
- An Injury Happens: If the patient, a family member, or even you get hurt in any way.
- A Medication or Care Error: If the wrong medicine is given, or if medicine is given at the wrong time or if there a different error in patient care.
- Behavior Changes: If the patient suddenly becomes very confused, angry, or upset.
- Safety Concerns: If something dangerous happens or almost happens, like if a patient tries to leave the house when they shouldn’t or if you feel uncomfortable or unsafe.
- Property Damage: If anything breaks or is damaged during the visit.
- Blood or Fluid Exposure: If you are exposed to blood or body fluids during the visit.
How to Write an Incident Report
- Write It Right Away: Write the report as soon as the incident happens. This way, the details are fresh in your mind.
- Stick to the Facts: Describe exactly what happened. Don’t guess or add your opinions. Just describe what you saw and heard.
- Be Specific: Include details like the time, place, and exactly what happened. If someone said something important, use their exact words.
- Report Injuries: If anyone was hurt, describe the injury and what was done to help.
- Include Witnesses: If someone else saw what happened, include their name and what they saw.
- Stay Calm: Use clear and simple words. Don’t blame anyone in the report, just describe what happened.
- Tell Your Supervisor: Always report the incident to your supervisor as soon as possible.
Why Incident Reports Matter
- Safety: Incident reports help keep patients and caregivers safe by making sure everyone knows about any problems or risk.
- Improvement: These reports help the care team learn from mistakes and prevent them from happening again.
- Legal Protection: Documenting incidents protects you and the agency by showing that you reported what happened.

by editor | Aug 11, 2024 | Care Keys - Aides
When you talk to a patient, you share information with them, and they share information with you. Communication can happen in many ways, such as:
- Talking
- Writing
- Pictures
- Drawing
- Actions
Understanding the Patient’s Emotions
- Empathy: Try to understand how the patient feels. Showing that you care can help build trust and make the patient feel calmer.
- Non-Verbal Communication: Pay attention to the patient’s body language, facial expressions, and actions, especially if they can’t talk.
Encouraging Communication
- Ask Simple Questions: Use simple yes/no questions or short sentences to help the patient express themselves.
- Repeat Back: To make sure you understood, repeat what the patient said in your own words.
Handling Difficult Behavior
Sometimes, patients might act in a way that seems angry or upset. They might hit, bite, push, yell, scream, or kick. Patients might do this because:
- They feel frustrated.
- They don’t feel well.
- It’s just part of their personality.
Remember, it’s not usually about you. The patient is likely reacting to how they feel. But it’s important to write down what happened and tell your supervisor. The care team needs to know about this behavior because it might show that the patient’s health is changing.
How to Respond When a Patient is Upset
- Protect Yourself: If the patient tries to hit or kick, block the blows or move out of the way. Never hit back.
- Give Them Time: Let the patient calm down before you try to talk to them again.
- Keep Them Safe: Make sure the patient is in a safe place.
- Give Them Space: Let the patient have some room and don’t crowd them.
- Stay Calm: Speak in a calm, quiet voice.
- Be Patient: Take your time and be flexible with the patient.
- Stay Neutral: Don’t argue or get into a fight with the patient. Stay calm, even if they say something mean.
- Use Gentle Movements: Don’t make sudden gestures or movements that might scare the patient.
- Be Supportive: Reassure the patient that you are there to help.
- Think About the Cause: Try to figure out what might have made the patient upset.
- Report the Behavior: Always tell your supervisor about any bad behavior so they can help.
Dealing with Non-Responsive Patients
- Gentle Encouragement: Some patients might not respond at all. Keep talking gently and offering encouragement. Even if they don’t answer, they might still hear you and feel comforted by your presence.
- Use of Familiar Items: Show the patient familiar objects like photos or favorite items. This can help them feel more at ease and might help them open up.
Involving the Family
- Family Support: Encourage family members to be part of the communication process when possible. They can often help calm the patient or provide important information about what might upset or comfort them.
Where Can You Find More Information

by editor | Aug 11, 2024 | Care Keys - Aides
Before you start taking care of a patient, follow these important steps. Doing them each time helps you remember and makes them a habit, ensuring both you and your patient are safe and comfortable.
1. Wash Your Hands:
Washing your hands helps stop the spread of germs and keeps everyone healthy. Many illnesses spread if hands are not washed properly. Always wash your hands before you start taking care of a patient.
How to Wash Your Hands:
- Soap and Water: If you have soap and water, scrub your hands with soap for at least 20 seconds. Make sure to wash all parts of your hands, including between your fingers and under your nails.
- Rinse: Rinse your hands with clean, running water.
- Hand Sanitizer: If soap and water are not available, use hand sanitizer with at least 60% alcohol. Rub it all over your hands until they are dry.
Tip: You might need to wash your hands more than once during patient care. Always wash before starting any new task.
2. Explain the Procedure to the Patient and Family
Tell the patient and their family what you are going to do. This helps them feel less worried and more willing to help.
How to Communicate:
- Speak Slowly: Use simple words that are easy to understand.
- Speak Clearly: Make sure your words are clear and easy to hear.
- Eye Contact: Look at the person you are talking to. This helps build trust and ensures they are listening.
Tip: Talking calmly and clearly can help reduce anxiety and make the procedure go more smoothly.
3. Give the Patient Privacy
Make sure the patient feels comfortable and respected by giving them privacy during care.
How to Provide Privacy:
- Close Curtains or Doors: Use curtains or doors to create a private space.
- Cover the Patient: Use sheets or blankets to cover the patient as needed.
Tip: Privacy helps the patient feel more at ease and respected during care.
4. Keep the Patient Safe
Ensure the patient is safe throughout the care process.
Safety Measures for Patients
- Adjustable Bed: If the patient is in a bed that can move, lower the bed to the lowest position and lock the wheels to prevent movement.
- Wheelchair: If the patient is in a wheelchair, lock the wheels to keep the chair stable.
Tip: Regularly check that the bed and wheelchair are in the correct position and locked properly.
5. Think About Your Safety
Your safety is also important. Proper positioning and adjustments help prevent injury.
Safety Tips for Caregivers:
- Adjustable Bed: Adjust the bed to a height that is comfortable for you to avoid bending or reaching awkwardly.
- Proper positioning: Make sure you are in a good position to avoid straining your back or hurting yourself. Use proper lifting techniques.
Tip: If the bed or chair needs to be adjusted, do so before starting the procedure to make it easier and safer for you.
Additional Tips
- Routine Checks: Regularly review these steps to ensure you are following them correctly.
- Ask for Help: If you are unsure about any procedure or need assistance, ask a supervisor or colleague.
Where Can You Get More Information
CDC Hand washing protocol

by editor | Aug 11, 2024 | Care Keys - Aides
It’s important to follow these steps after you finish taking care of a patient. Doing these steps every time helps you remember them and makes them a habit. This helps keep both you and your patients safe and healthy.
1. Lower the Patient’s Bed
If you raised the bed to take care of the patient, be sure to lower it back down to its lowest position. This helps prevent falls and keeps the patient safe.
Tip: Always check that the bed is locked in place after lowering it.
2. Wash Your Hands
Washing your hands stops the spread of germs and helps keep everyone healthy. Always wash your hands after finishing any patient care.
How to Wash Your Hands:
- Soap and Water: Scrub your hands with soap for at least 20 seconds. Make sure to wash all parts of your hands, including between your fingers and under your nails.
- Rinse: Rinse your hands with clean, running water.
- Hand Sanitizer: If soap and water aren’t available, use hand sanitizer with at least 60% alcohol. Rub it all over your hands until they are dry.
3. Write Down What You Did
Take notes about the care you provided, how the patient is doing, and any important information about the family or caregiver. Writing down what you did helps ensure the patient gets the best care.
Why It’s Important:
- Communication: Your notes help the healthcare team understand the patient’s condition and decide if any changes are needed in their care.
- Quality of Care: Detailed notes ensure the patient receives consistent and high-quality care.
- Legal Requirement: Accurate documentation is required by law. If you don’t record what you did, it’s as if the care never happened.
How to Document:
- Be Detailed: Write clearly about the care provided and any changes in the patient’s condition.
- Include Quotes: If the patient or family member says something important, use quotation marks to note their exact words.
Additional Tips:
- Double-Check: Before leaving, make sure the bed is in the correct position and locked, and confirm that all documentation is complete.
- Consistency: Make these steps a routine part of your care process to ensure nothing is missed.

by editor | May 10, 2024 | Hospice 101 - Aides, Hospice 101 - Chaplain, Hospice 101 - Nurses, Hospice 101 - Social Workers, Resources and Readings
Caregivers play a critical role in hospice care, where the focus is on providing comfort and support to individuals nearing the end of life. These unsung heroes, often family members or close friends, offer physical, emotional, and spiritual support to their loved ones during one of life’s most challenging transitions. However, the demands of caregiving can take a toll, leading to burnout and reduced well-being. Recognizing and addressing caregiver burnout is essential for ensuring ongoing support for patients and their families.
Understanding Caregiver Burnout:
Caregiver burnout is a multifaceted phenomenon that is characterized by physical, emotional, and mental exhaustion. It can manifest as feelings of overwhelming stress, compassion fatigue, depression, and a sense of hopelessness. According to the Mayo Clinic, symptoms of burnout may include fatigue, irritability, withdrawal from social activities, and a lack of motivation or interest in caregiving tasks. If caregiver burnout is not addressed, it can have a negative impact on the quality of care provided to patients and negatively impact caregivers’ own health and well-being.
Research conducted by the Ann & Robert Lurie Children’s Hospital of Chicago and the University of Pittsburgh sheds light on the prevalence and impact of caregiver burnout in hospice settings. Dr. Michael Certo, assistant professor of pediatrics at Lurie, emphasizes the high risk of emotional, social, and financial consequences for caregivers. The study found that caregiver burnout is alarmingly common among those providing end-of-life care, underscoring the need for targeted interventions and support mechanisms.
Assessing Caregiver Distress:
To effectively address caregiver burnout, healthcare providers must first identify individuals at risk. The research team implemented a standardized method for assessing caregiver distress, recognizing the importance of early intervention in mitigating burnout. The caregiver self-assessment questionnaire, developed by the American Geriatric Society, emerged as a valuable tool for screening caregivers’ well-being. This brief yet comprehensive metric enables clinicians to identify signs of burnout and tailor support interventions accordingly.
Supporting Caregivers:
Once caregiver distress is identified, healthcare providers can offer a range of supportive measures to promote resilience and well-being. These may include encouraging caregivers to prioritize self-care, providing access to respite care services, facilitating peer support groups, and connecting caregivers with community resources. Additionally, caregivers may benefit from educational programs aimed at enhancing coping skills, stress management techniques, and communication strategies.
The Impact of Caregiver Burnout on Hospice Care:
Caregiver burnout not only affects individual caregivers but also has broader implications for hospice care delivery. Research has shown that patients who do not have adequate caregiver support may be less likely to choose hospice care, leading to delayed referrals and suboptimal end-of-life experiences. Moreover, caregiver burnout can strain healthcare resources and contribute to caregiver turnover, compromising the continuity and quality of care provided to patients and families.
Addressing the Financial Burden:
In addition to the emotional and physical toll, caregiving often imposes a significant financial burden on families. According to AARP, unpaid family caregivers in the United States collectively spend billions of dollars annually on caregiving-related expenses. These costs may include medical bills, prescription medications, home modifications, and lost wages due to missed workdays. Recognizing the financial challenges faced by caregivers is essential for implementing policies and programs aimed at alleviating economic strain and promoting financial security.
In conclusion, caregiver burnout poses a significant challenge in hospice care, impacting both caregivers and the patients they serve. By implementing comprehensive assessment tools, providing targeted support interventions, and addressing the financial burdens associated with caregiving, healthcare providers can foster resilience and well-being among caregivers. Nurturing caregivers not only enhances the quality of care provided but also ensures that patients and families receive the compassionate support they need during life’s final journey.
Where Can you Get Additional Information:
- Mayo Clinic. (n.d.). Job burnout: How to spot it and take action. Retrieved from Mayo Clinic
- National Institute on Aging. (n.d.). Taking Care of Yourself as a Caregiver. Retrieved from National Institute on Aging
- AARP Public Policy Institute. (2021). Family Caregiving and Out-of-Pocket Costs: 2016 Report. Retrieved from AARP Public Policy Institute
- American Geriatrics Society. (n.d.). Caregiver Self-Assessment Questionnaire. Retrieved from American Geriatrics Society
- Hospice Foundation of America. (n.d.). Caregiving at the End of Life: Finding Resilience. Retrieved from Hospice Foundation of America
- Morrison, R.S. et al. (2009). Palliative Care Consultation Teams Cut Hospital Costs for Medicaid Beneficiaries. Health Affairs, 28(3), w450-w460. Retrieved from Health Affairs